Gut:重磅!伦敦癌症研究中心科学家找到食管癌的软肋,有望拯救近半数的食管癌患者
2017-08-28 朱爽爽 奇点网
8月22日,来自伦敦癌症研究所Christopher Lord教授的科研团队在胃肠病领域顶级期刊《Gut》杂志上刊登了一项关于食管癌治疗的突破性发现(1),他们可能找到了食管癌的软肋。
8月22日,来自伦敦癌症研究所Christopher Lord教授的科研团队在胃肠病领域顶级期刊《Gut》杂志上刊登了一项关于食管癌治疗的突破性发现(1),他们可能找到了食管癌的软肋。
他们发现,通过使用小分子干扰RNA抑制靶向Bruton酪氨酸激酶(BTK)的活性,可以显著抑制MYC/ERBB2基因活性上调的食管癌细胞的增殖。同时,研究人员还发现,目前FDA已经批准的用于治疗多种癌症的BTK抑制剂ibrutinib,同样可以显著抑制食管癌细胞的增殖,并且与小分子干扰RNA活性相当。
由于近半数的食管癌患者体内都会出现MYC/ERBB2基因活性上调(2)。这意味着,近半数的食管癌患者将有望从这一发现中受益。

Lord教授
食管癌是一种在发展中国家属常见肿瘤,我国更是食管癌发生大国。2014年世界卫生组织的统计资料显示,我国食管癌患者人数已经占到了全球患者的一半,同时,全球近45万死亡病例中,有49%发生在我国(3)。特别地,河南、四川、福建和广东等都是我国食管癌高发地区,河南安阳、河北邯郸以及晋东南地区食管癌死亡率常年居高不下。
而由于食管癌侵袭性特别强,大多数患者确诊时就已经是中、晚期了,无法进行手术治疗。而就算有小部分患者可以进行手术治疗,食管癌术后的复发率也非常高。此外,除了手术之外,食管癌目前可用的临床治疗方案非常有限。因此,食管癌患者总体的5年生存率只有19%(4)。
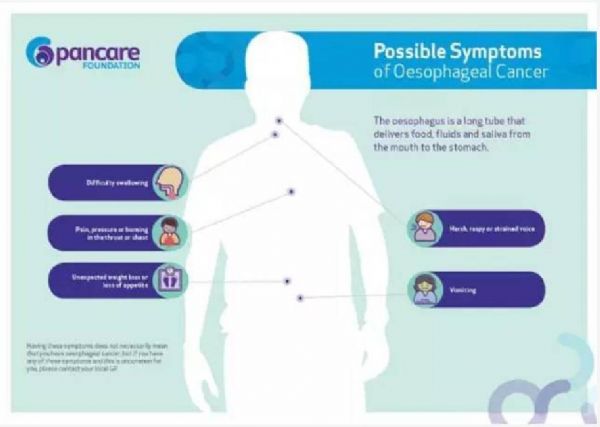
食管癌常见的临床症状
食管癌可以分为食管腺癌(EAC)以及食管鳞癌(ESCC)两大类。目前对于EAC的治疗有基于顺铂,紫杉烷类,喜树碱类的化疗。同时,化疗无效的EAC患者还有一些靶向药物可以选择,例如靶向抗血管内皮生长因子受体的ramucirumab,尽管这些治疗方案的效果并不是很好(5)。
而对于ESCC,除了化疗之外目前还没有靶向药物被批准用于ESCC的治疗。也就是说,一旦一线化疗方案失败,将没有任何治疗方案可供ESCC患者选择。但是,偏偏90%的食管癌患者都属于ESCC(3)。因此,寻找食管癌治疗新方案是非常必要的,尤其对那些无药可用的ESCC患者。
Lord教授长期致力于食管癌的研究。而为了找到合适的治疗食管癌的药物,Lord教授的想法非常“简单粗暴”。既然,癌细胞是由基因突变产生的,同时,癌细胞的生长增殖往往很依赖于某些活性上调的基因,即促癌基因,而正常的细胞不会。那么,这些癌细胞所依赖的基因,以及其控制的下游通路同时也是治疗癌症很有希望的靶点。

而为了找到这些潜在的靶点,Lord教授的做法更加“简单粗暴”。首先,Lord教授选择了17种常见的食管癌细胞系(包括8中EAC细胞系以及9种ESCC细胞系)进行实验。收集了这17种常见的食管癌细胞的基因数据,并按癌细胞内促癌基因的类型进一步将这些细胞分类。例如,MYC基因活性上调的癌细胞归为一类。
随后,Lord教授直接用80种临床上常用的或者处于研发后期的抗癌药物来处理这些细胞(这些药物的作用靶点是完全不同的),以收集不同类型的食管癌细胞对于这些药物的敏感性数据。同时,Lord教授还找到了714种已知的靶向与癌症相关激酶的小分子干扰RNA(6),同样用这些小分子干扰RNA处理所有不同类型的细胞,以收集癌细胞对这些激酶调控的基因的依赖性数据。
通过整合这些数据Lord教授发现,常见的促癌基因MYC活性上调的食管癌细胞对于靶向布BTK的小分子干扰RNA异常敏感。靶向BTK的小分子干扰RNA可以显著抑制MYC基因活性上调癌细胞的生长增殖。
由于FDA已经批准BTK抑制剂ibrutinib用于多种的癌症治疗(7,8),同时,已知ibrutinib还能直接抑制促癌基因ERBB2的活性(9)。因此Lord教授便同时测试了ibrutinib对于MYC以及ERBB2基因活性上调的食管癌细胞的效果。
结果,Lord教授惊喜的发现,ibrutinib与靶向BTK的小分子干扰RNA效果相似,同样可以显著抑制MYC基因活性上调食管癌细胞的生长增殖。不仅如此,对于ERBB2基因上调的食管癌细胞,ibrutinib同样有效。
最后,研究人员还发现了ibrutinib抑制MYC或者ERBB2基因上调癌细胞的机制。ibrutinib可以选择性诱导MYC以及ERBB2基因活性上调的癌细胞在有丝分裂时,停止在G1期,随后引发癌细胞凋亡,从而发挥抗癌作用。

由于ibrutinib此前已经被FDA批准用于其他类型癌症的治疗。所以ibrutinib的安全剂量范围是已知的。因此,Lord教授已经开始进行二期临床试验,进一步验证ibrutinib对于MYC以及ERBB2基因活性上调患者的有效性。
同时,此前的研究表明,ERBB2基因在11%的ESCC患者以及32%的EAC患者中活性显著上调。而MYC基因活性同样在23%的EAC患者以及32%的ESCC患者体内上调(2)。这意味着,一旦ibrutinib在人体实验中被证明有效,那么近半数的食管癌患者将会从中受益。

总的来说,这一发现无疑是非常重要的。此前研究表明,无论是化疗还是仅有的针对EAC的靶向治疗,患者的无进展生存期都在7个月左右(10)。因此,大部分患者在治疗过程中会经历癌症的复发。而此时,占比90%的ESCC患者已经无药可用。这也可能是食管癌5年生存率如此低的一个重要原因。我们也期待ibrutinib能在针对食管癌的二期临床中取得良好效果。
参考资料:
1.Irene Yushing Chong1, Lauren Aronson, Hanna Bryant,et al.Mapping genetic vulnerabilities reveals BTK as a novel therapeutic target in oesophageal cancer . doi: 10.1136/gutjnl-2017-314408
2.Cancer Genome Atlas Research Network. Integrated genomic characterization of oesophageal carcinoma[J]. Nature, 2017, 541(7636): 169-175.
3.World Cancer Report 2014[M]. World Health Organization, 2014.
4.Rustgi A K, El-Serag H B. Esophageal carcinoma[J]. New England Journal of Medicine, 2014, 371(26): 2499-2509.
5.Pozzo C, Barone C, Szanto J, et al. Irinotecan in combination with 5-fluorouracil and folinic acid or with cisplatin in patients with advanced gastric or esophageal-gastric junction adenocarcinoma: results of a randomized phase II study[J]. Annals of Oncology, 2004, 15(12): 1773-1781.
6.Campbell J, Ryan C J, Brough R, et al. Large-scale profiling of kinase dependencies in cancer cell lines[J]. Cell reports, 2016, 14(10): 2490-2501.
7.Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med 2013;369:32–42.
8.Wang ML, Rule S, Martin P, et al. Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med 2013;369:507–16.
9.Grabinski N, Ewald F. Ibrutinib (ImbruvicaTM) potently inhibits ErbB receptor phosphorylation and cell viability of ErbB2-positive breast cancer cells. Invest New Drugs 2014;32:1096–104.
10.Bang Y J, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial[J]. The Lancet, 2010, 376(9742): 687-697.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#食管癌患者#
54
非常好的文章.学习了非常好的文章.学习了
103
谢谢分享.学习了!
102
#食管#
60
#癌症研究#
72
#重磅#
62
非常好的文章.学习了非常好的文章.学习了
96