化疗是最好的治癌方法吗?来自纽约理工学院的研究人员为正在接受化疗的患者找到了更有效的治疗手段。
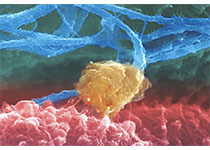
《美国国家科学院学报》中发表了来自于纽约理工学院生物医学科学博士的研究报告,在此次报告中,研究人员记录了详细的研究结果,表明全新合成的相互作用可以在间充质细胞抑制肿瘤的生长,间充质细胞指的是细胞发展成结缔组织,如骨头,软组织和中枢神经系统。
化疗会伤害健康细胞,带来不愉快的副作用,如脱发和呕吐。然而,化疗是目前唯一可用的持续治疗替代延长端粒(ALT)癌症的方法,尽管ALT癌细胞仅占所有癌症病例的10%至15%,但是其中却包括非常知名的癌症,如胶质母细胞瘤。
研究人员试图找到抑制ALT癌症的生长的最佳方法,因为他们一直在寻求潜在的新疗法。为此他们调查了三个相关的人类基因癌症发展,即FANCM(突变有关血液癌症),BRCA1(突变的患者常见乳腺癌和卵巢癌)和BLM(导致各种癌症的基因突变)。当BRCA1或BLM的细胞不足时,FANCM修复两个错误联系的DNA链,因此,研究小组发现,同时失活BLM FANCM和BRCA1,FANCM会戏剧性的增加未修理的受损DNA,防止癌变细胞进一步繁殖。
这些发现表明,如果新开发的药物可以同时抑制BLM和FANCM,或BRCA1和FANCM,他们应该杀死ALT癌症,并且可以摆脱传统化疗药物的毒性作用。
原始出处:
Pan X, Drosopoulos WC, Sethi L, et al.FANCM, BRCA1, and BLM cooperatively resolve the replication stress at the ALT telomeres.Proc Natl Acad Sci U S A. 2017 Jul 18;114(29):E5940-E5949. doi: 10.1073/pnas.1708065114. Epub 2017 Jul 3.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#研究人员#
48
#癌症治疗#
66
#新突破#
65
#PNAS#
58