一例直肠医源性穿孔的处理体会
2018-05-29 佚名 “华亭论镜”公众号
患者,女性,54岁,因“便秘10余年”就诊我科,既往有剖宫术史。为了解患者便秘原因,行结肠镜检查,检查过程中,发现患者乙状结肠冗长,进镜过程起袢明显,推镜中患者出现肛门流血,即予退镜观察,于距离肛门口约4cm处直肠前壁见一撕裂性穿孔,约2.5×3.5cm。
病例资料
患者,女性,54岁,因“便秘10余年”就诊我科,既往有剖宫术史。为了解患者便秘原因,行结肠镜检查,检查过程中,发现患者乙状结肠冗长,进镜过程起袢明显,推镜中患者出现肛门流血,即予退镜观察,于距离肛门口约4cm处直肠前壁见一撕裂性穿孔,约2.5×3.5cm。面对这么大的直肠穿孔,我们未曾遇到,情况较为急迫,患者面临伤口、腹膜后乃至腹腔感染的风险。我们迅即制定了治疗策略:减少伤口的进一步污染,封闭创面,抗感染治疗,密切观察。于是,调整患者体位,将伤口摆放至肠腔的高位,防止肠内容物流入伤口;伤口较大,一般金属夹缝合法无法封闭创面,故选择应用荷包缝合法(参见图1及视频),操作过程顺利,创面得到完全封闭;留置肛管,禁食、静脉应用广谱抗生素。术后当天患者体温上升至39度,查体:腹软,下腹压痛,无反跳痛,血白细胞升高至21×10^9/L,行腹部CT提示腹膜后及腹腔大量气体。次日复查内镜显示创面封闭良好。继续抗感染治疗数天后,患者症状逐渐缓解,1周后痊愈出院。
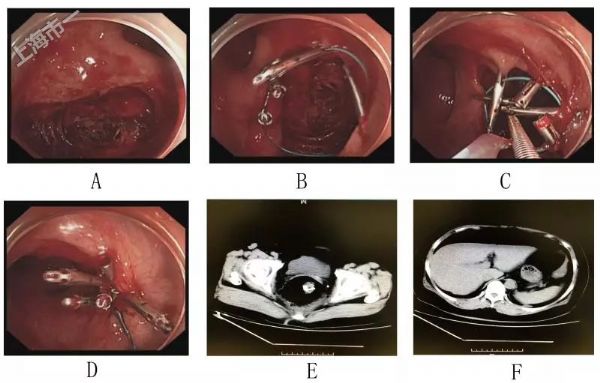
图1 A-D:直肠穿孔荷包缝合的过程;E-F:穿孔当日CT提示直肠周围、腹膜后及腹腔积气
讨论
常规内镜检查中并发直肠穿孔比较少见,但一旦发生,对内镜医生是一个较大的挑战。针对该例患者的处理,我们有以下几点体会:
1. 良好的肠道准备,不但是检查顺利进行的基础,也是并发症发生后能妥善处理的关键。直肠部位细菌含量高,发生穿孔后极易并发感染,该患者肠道准备佳,对于避免伤口、腹膜后及腹腔的感染至关重要。
2. 结肠镜检查前及检查中应对患者的操作难度有准确评估,如出现操作困难,应及时中止检查或交给更有经验的医生。该患者为中年女性,长期便秘,乙状结肠冗长,有剖宫术史,均为困难操作的提示点。
3. 一旦并发穿孔,应冷静对待,及时制定合适处理策略。该部位穿孔外科治疗常较为棘手,应争取内镜下处理。首先应即刻调整体位,将伤口摆放至肠腔的高位,避免创面的进一步污染。接下选择合适方式封闭伤口是治疗过程的关键,可根据伤口情况应用金属夹或荷包缝合法封闭创面。封闭创面后留置肛管,可减少肠内容物对伤口的影响。
4. 直肠部位穿孔常难于避免并发感染,应即应用广谱抗生素。密切观察患者病情,直肠不同部位穿孔临床表现差异较大,如腹膜反折(约在距肛门口7cm,中直肠横襞处)以下直肠穿孔,腹肌紧张、压痛及反跳痛等腹膜炎表现可不明显,主要表现为直肠周围、盆腔的感染;而在腹膜反折以上直肠穿孔,常表现为腹膜炎体征。该患者穿孔部位主要在腹膜反折以下,同时可能局部腹膜有一定程度撕裂,故腹膜炎体征不明显,同时腹腔内也可见游离气体。
5. 病情观察过程中,可行结肠镜及影像学复查,如出现伤口开裂,腹膜后渗出进行性加重乃至脓肿形成,应请外科进行处理。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了.谢谢作者分享!
98
学习了.谢谢作者分享!
108
#穿孔#
91
好文献.学习了
97
学习了
98