J Rheumatol: OMERACT拇指基部骨关节炎磁共振成像评分系统(TOMS)的纵向可靠性
2018-12-22 xiangting MedSci原创
TOMS的纵向可靠性为中等至良好。很少有变化阻碍评估。
这项研究旨在评估风湿病结果测量(OMERACT)拇指基部骨关节炎磁共振成像(MRI)评分系统(TOMS)的纵向可靠性。
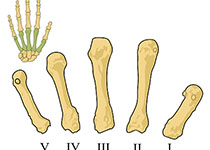
对手部骨关节炎患者2次运动时(6个月和2年随访)的配对MRI进行评分,评分内容包括滑膜炎、软骨下骨缺损(SBD)、骨赘、软骨评估、骨髓病变(BML)和半脱位。评估了阅片者间可靠性的δ评分。
很少有变化出现。除了滑膜炎(0.55-0.83)和腕掌-1骨赘/软骨评估(0.47/0.39)以外,平均测量组内相关系数良好(≥0.71)。除了2年BML以外(28%/64-76%),精确/密切一致性的百分比为52-92%/68-100%。除SBD和BML外,最小的可检测变化低于评分增量。
TOMS的纵向可靠性为中等至良好。很少有变化阻碍评估。
原始出处:
Féline P.B. Kroon. Longitudinal Reliability of the OMERACT Thumb Base Osteoarthritis Magnetic Resonance Imaging Scoring System (TOMS). J Rheumatol. 15 December 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#骨关节#
87
#磁共振成像评分系统#
72
#ERA#
70
#关节炎#
74
#磁共振#
79
学习了
87