Gynecol Oncol:宫颈病变LEEP和激光锥切术复发率:5年随访研究结果
2021-09-22 王晨 张师前 张师前公众号
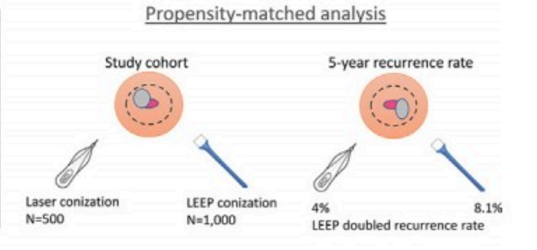
比较激光锥切术和环形电切术(LEEP)在高度宫颈上皮内瘤变(HSIL/CIN2+)患者中的复发率。方法:收集2010年至2014年接受锥切手术的HSIL/CIN2+患者的诊疗数据。采用倾向评分匹配(P
摘要
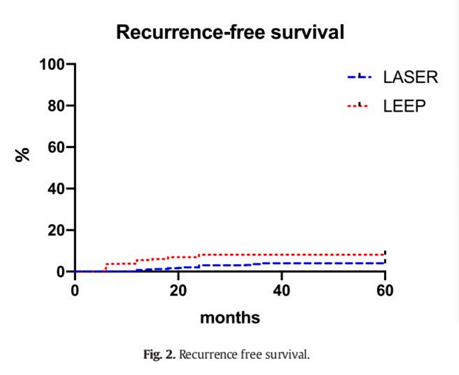
目的:比较激光锥切术和环形电切术(LEEP)在高度宫颈上皮内瘤变(HSIL/CIN2+)患者中的复发率。方法:收集2010年至2014年接受锥切手术的HSIL/CIN2+患者的诊疗数据。采用倾向评分匹配(PSM)以减少分配偏差。Kaplan-Meir和Cox风险模型估计复发风险。结果:2966例锥切患者中,567例接受(20%)激光锥切,2399例(80%)LEEP手术。CIN3(HR:3.80(95%CI:2.01,7.21);p<0.001)和HPV持续性感染(HR:1.81 (95%C1:1.11,2.96);P < 0.001)与复发风险增加相关。选择500例接受激光锥切患者和1000名接受LEEP的患者进行(1:2)PSM匹配,发现LEEP手术切缘阳性的风险更高(11.2% vs. 4.2%)。两组患者HPV持续感染的风险相似(15.0% vs. 11.6%;p = 0.256)。LEEP术后5年复发率为8.1%,激光锥切术后5年复发率为4% (p = 0.023)。结论:HPV持续感染是激光锥切术或LEEP术后复发风险增加的最主要相关因素。
方法
入组标准:新诊断的中/重度宫颈上皮内瘤变(HSIL/CIN2+);鳞状细胞癌。排除标准:年龄< 18岁;有消融及冷刀锥切史;腺体病变;妊娠期;有子宫切除术史。
患者锥切术后3个月(阳性切缘)/ 6个月(阴性切缘)门诊进行阴道镜检查。后期随访时间为:前两年每6个月1次,之后每年1次,直到5年。HPV持续感染定义为在锥切术后第一次临床检查中检测到的HPV(通常在6个月)。复发性宫颈上皮内瘤变定义为患者在锥切与HSIL/CIN2+诊断之间至少有一次阴性检查。低级别宫颈病变(LSIL/CIN1)不被认为是复发性疾病。
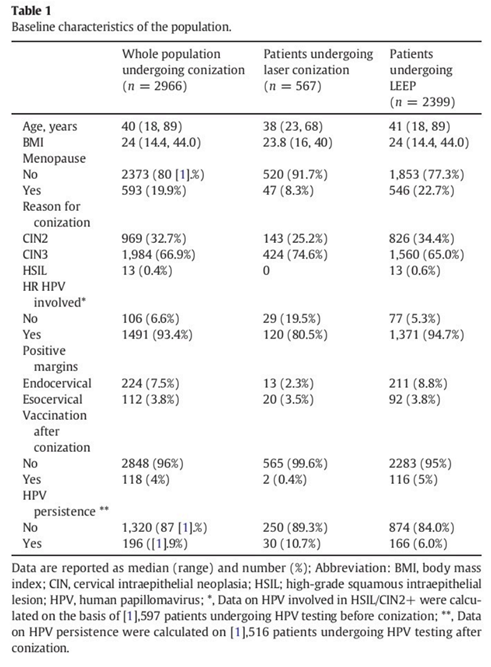
鉴于两组之间的回顾性比较,进行倾向评分分析(PSM),目的是减少来自不同协变量的偏倚。开发多变量logistic回归模型。年龄、病变类型(CIN2 vs. CIN3)、绝经状态、锥切前是否进行HPV检测。激光锥切术与LEEP患者的比例为1:2,P值<0.05有统计学意义。
结果
175例患者初次治疗之后的5年内复发,复发率为6%,复发中位时间18个月(5-32月)。LEEP组155例(6.4%),激光锥切组20例(3.5%)(P=0.0007),两年内复发率占5%,在3-5年内复发占1%。
单因素分析:宫颈上皮内瘤变(HR: 1. 68 (95%CI:1. 21, 2. 33) /CIN3;p=0. 002)、术前检测的HR HPV 类型(HR : 2.69 (95%CI: 1.25, 5.81); p= 0.011),、手术切缘阳性(HR: 2.44 (95% CI:1.68, 3. 55) ; p< 0.001)、 HPV 持续感染(HR:2. 34 (95% CI: 1. 64, 3. 33) ; p< 0. 001)和手术方式(HR: 2. 50 (95%CI: 1.99, 3.16) ; p= 0. 007)。
多因素分析中:CIN3 (HR: 3.80 (95%CI: 2.01, 7.21);p< 0.001)和HPV持续性感染(HR: 1.81 (95%CI: 1.11, 2.96);P<0.001)与复发风险相关。尽管手术方式虽无统计学意义,但与复发风险略有相关(HR: 1.28 (95%CI:0.78, 2.69);p = 0.071)。
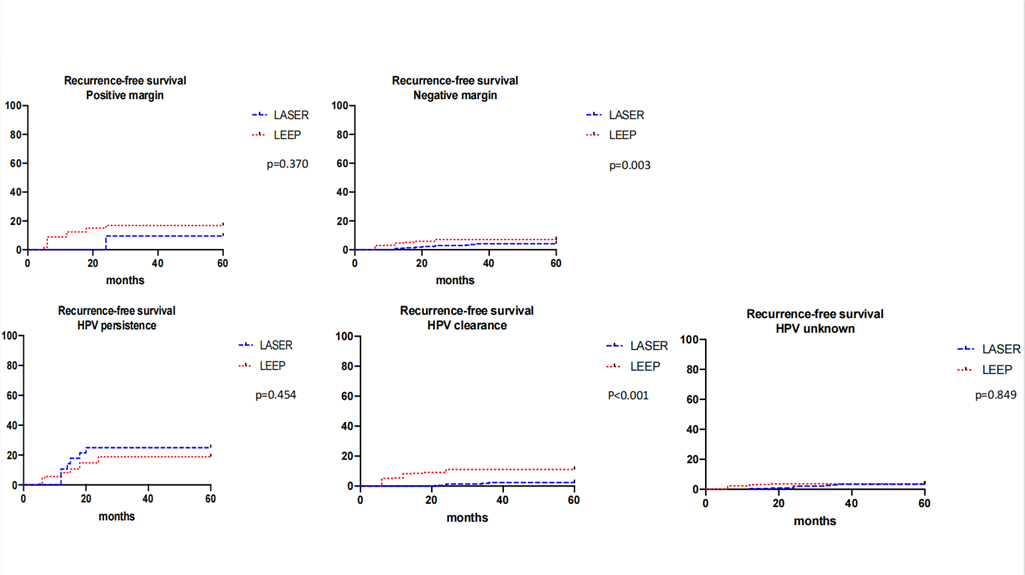
激光锥切后,HPV持续感染是影响复发的主要因素,此外,术后切缘阳性对复发也有一定的影响;LEEP术后,CIN3 (HR: 3.48 (p= 0.001)、切缘阳性(p= 0.001)和HPV持续性感染(p= 0.001)与复发有相关关系。
讨论
本研究报道宫颈上皮内瘤变(HSIL/CIN2+)患者经LEEP和激光锥切术后的复发率。本回顾性研究收集了3000例接受锥切手术的患者的数据,进行了5年随访。是调查不同手术方式对宫颈上皮内瘤变患者锥切影响的最大研究。为了减少可能的分配偏差,采用了倾向评分算法。发现:1.无论手术方式如何,HPV持续感染是增加复发风险的最主要因素;2.与LEEP相比,激光锥切术后HSIL/CIN2+的复发风险较低;3.激光锥切术后阳性切缘(特别内切缘)发生率低于LEEP,HPV持续感染不受手术方式的影响。4.阳性切缘是LEEP后复发的重要危险因素,而在激光锥切组中,未观察到阳性切缘与复发率之间的关系。
原始出处:
Recurrence rate after loop electrosurgical excision procedure (LEEP) and laser Conization: A 5-year follow-up study.Gynecol Oncol. 2020 Dec;159(3):636-641. doi: 10.1016/j.ygyno.2020.08.025
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#宫颈锥切技术##LEEP刀#
48
#宫颈病变#
50
#NEC#
42
#复发率#
55
#Oncol#
38
#随访研究#
49
#研究结果#
38
#5年随访#
0
#激光#
35
#宫颈#
43