Ann Rheum Dis:炎症性关节病和DMARD治疗患者的流感结局
2021-11-25 MedSci原创 MedSci原创
从绝对值来看,IJD患者的COVID-19病例数量超过平均季节性流感,但IJD导致两种感染的住院和死亡风险分别增加50%-100%,这在很大程度上取决于相关的合并症。
近日,风湿病领域顶级期刊Annals of the Rheumatic Diseases上发表了一篇研究文章,该研究旨在评估炎症性关节病(IJD)和接受缓解疾病的抗风湿药治疗(DMARD)的患者季节性流感结局的绝对和相对风险,并将最近关于相应COVID-19风险的研究结果汇总起来。

在这项队列研究中,研究人员使用瑞典全国登记中心随访了116989名IJD患者和匹配的人群对照者,受试者跨越了四个流感季节(2015-2019年)。

研究人员量化了因流感住院和死亡的绝对风险,并通过Cox回归将IJD患者与对照者进行了比较。在每个流感季节开始时,研究人员确定了71556名接受常规合成DMARDs和生物疾病缓解抗风湿药物(bDMARDs)/靶向合成疾病缓解抗风湿药物(tsDMARDs)积极治疗的IJD患者,并估计相同结局的风险,以及通过Cox回归比较了不同DMARD组别的这些风险。
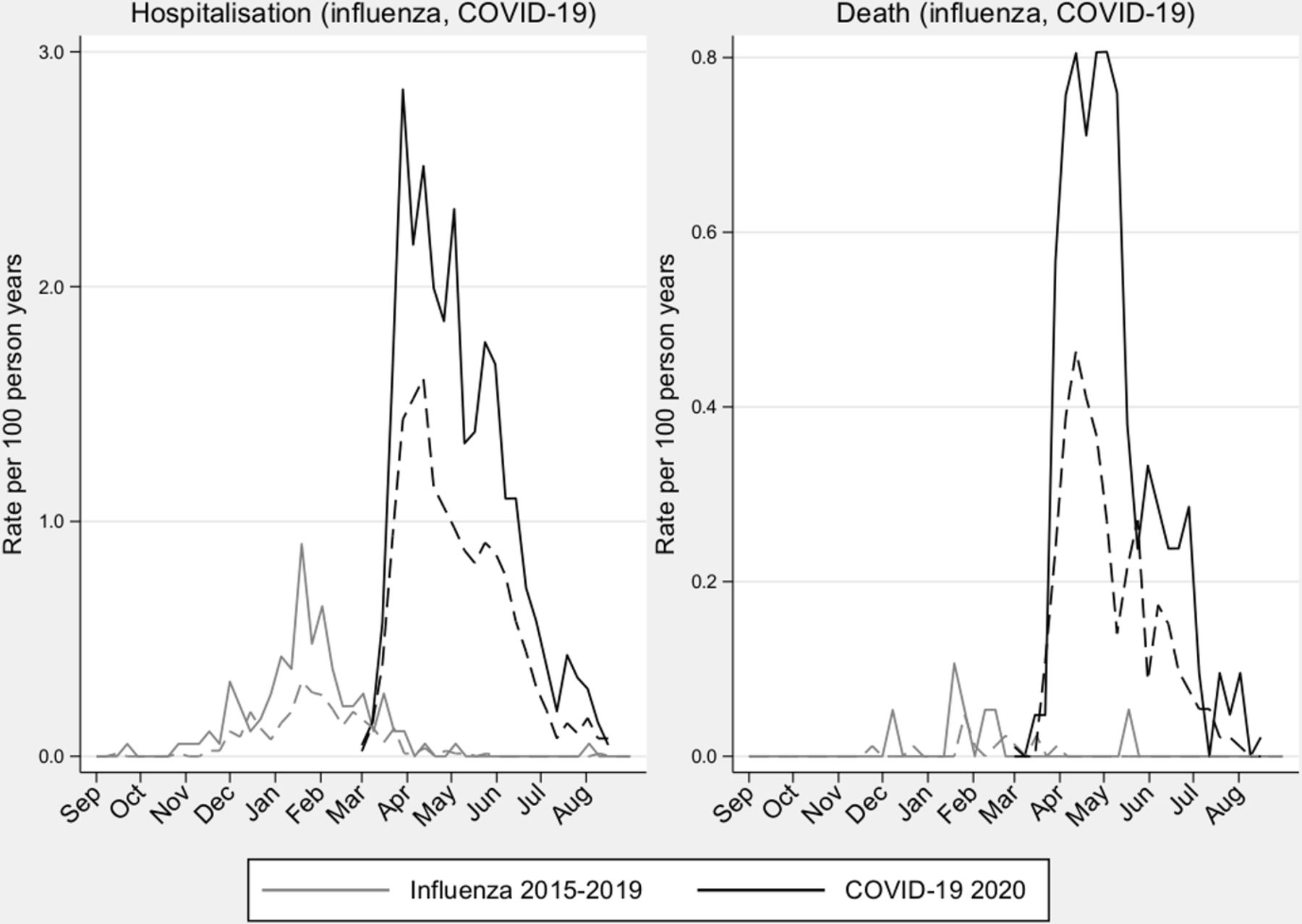
每个季节,IJD患者因流感住院的平均风险为0.25%,一般人群为0.1%,对应的粗略的HR为2.38(95%CI为2.21至2.56),并对合并症进行调整后,下降至1.44(95%CI为1.33至1.56)。对于列入死亡名单的流感,相应的数字分别为0.015%和0.006%(HR=2.63,95%CI为1.93至3.58,HR=1.46,95%CI为1.07至2.01)。流感结局的绝对风险是COVID-19的一半(住院)和十分之一(死亡),但将IJD患者与一般人群进行比较的相对估计值类似。
由此可见,从绝对值来看,IJD患者的COVID-19病例数量超过平均季节性流感,但IJD导致两种感染的住院和死亡风险分别增加50%-100%,这在很大程度上取决于相关的合并症。总体而言,bDMARDs/tsDMARDs治疗似乎不会增加与季节性流感相关的住院或死亡风险。
原始出处:
Hannah Bower,et al.Influenza outcomes in patients with inflammatory joint diseases and DMARDs: how do they compare to those of COVID-19?.Ann Rheum Dis.2021.https://ard.bmj.com/content/early/2021/11/21/annrheumdis-2021-221461
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Dis#
77
#炎症性#
54
#DMARD#
85