Onco Targets Ther:研究发现lncRNA LEF1-AS1或是治疗胶质母细胞瘤的关键
2017-09-24 MedSci MedSci原创
研究已经证实胶质母细胞瘤(GBM)组织中长链非编码RNA(lncRNA)是不同细胞过程的关键调节剂。然而,lncRNA的表达模式和生物学功能在很大程度上是未知的。在这里,研究人员首次探究了lncRNA淋巴增强子结合因子1反义RNA 1(LEF1-AS1)在体外和体内对GBM进展的影响。研究人员通过生物信息学分析研究了GBM标本中LEF1-AS1的表达谱。使用定量聚合酶链反应检测GBM组织中的LEF
研究已经证实胶质母细胞瘤(GBM)组织中长链非编码RNA(lncRNA)是不同细胞过程的关键调节剂。然而,lncRNA的表达模式和生物学功能在很大程度上是未知的。在这里,研究人员首次探究了lncRNA淋巴增强子结合因子1反义RNA 1(LEF1-AS1)在体外和体内对GBM进展的影响。
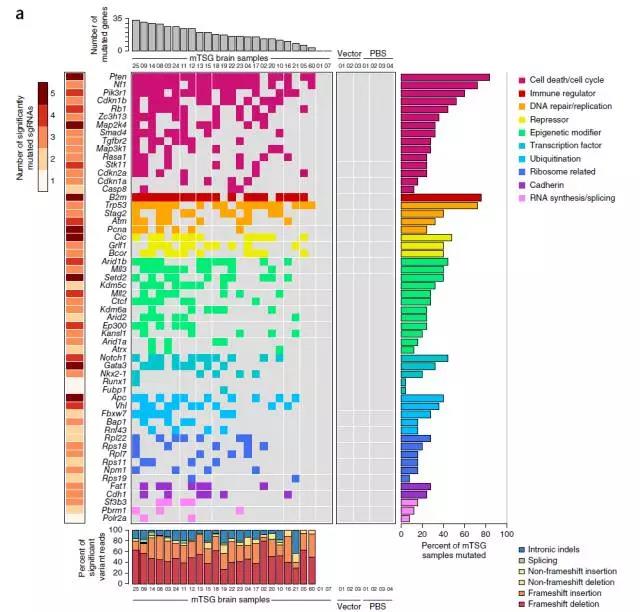
研究人员通过生物信息学分析研究了GBM标本中LEF1-AS1的表达谱。使用定量聚合酶链反应检测GBM组织中的LEF1-AS1表达。通过转染LEF1-AS1特异性小干扰RNA(siRNA)抑制LEF1-AS1的表达,并通过转染si-LEF1-AS1病毒抑制稳定细胞系。使用细胞计数试剂盒-8,乙炔基脱氧尿苷和集落形成法检测细胞的增殖功能。流式细胞术用于检测细胞周期变化和细胞凋亡。通过Transwell测定法检测细胞的迁移效应。使用肿瘤异种移植物和免疫组织化学以评价体内肿瘤的生长。
结果显示,与正常组织相比,GBM样本中LEF1-AS1的表达显著上调。来自LEF1-AS1高表达的癌症基因组图谱的GBM患者的5年总体生存率低于低表达者。GBF组织中LEF1-AS1的表达高于正常组织。敲除LEF1-AS1可显著抑制GBM细胞的恶性表现,包括细胞的增殖和侵袭,并可促进细胞凋亡。Western blot分析结果表明,敲除GBM细胞中LEF1-AS1介导的肿瘤抑制或是通过降低ERK和Akt / mTOR信号传导活性的而实现。最后,体内实验也证明,敲除LEF1-AS1可抑制U87细胞LEF1-AS1的生长促进作用。
总之,该结果表明,lncRNA LEF1-AS1作为GBM的一种癌基因,或是治疗这种疾病的关键点。
原始出处:
Jin Wang, Xiaoyang Liu, et al., LEF1-AS1, a long-noncoding RNA, promotes malignancy in glioblastoma. Onco Targets Ther. 2017; 10: 4251–4260. Published online 2017 Aug 28. doi: 10.2147/OTT.S130365
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#母细胞瘤#
57
#胶质母细胞#
49
#CRN#
55
#target#
65
#研究发现#
65
学习了.谢谢分享
99
#lncRNA#
65
#细胞瘤#
53