Leukemia:科学家发现WT1-MEG3信号通路有望成为治疗AML的新靶点
2017-12-22 MedSci MedSci原创
WT1-MEG3轴能抑制肿瘤生长,有望成为有效的治疗AML的一系列潜在的靶点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

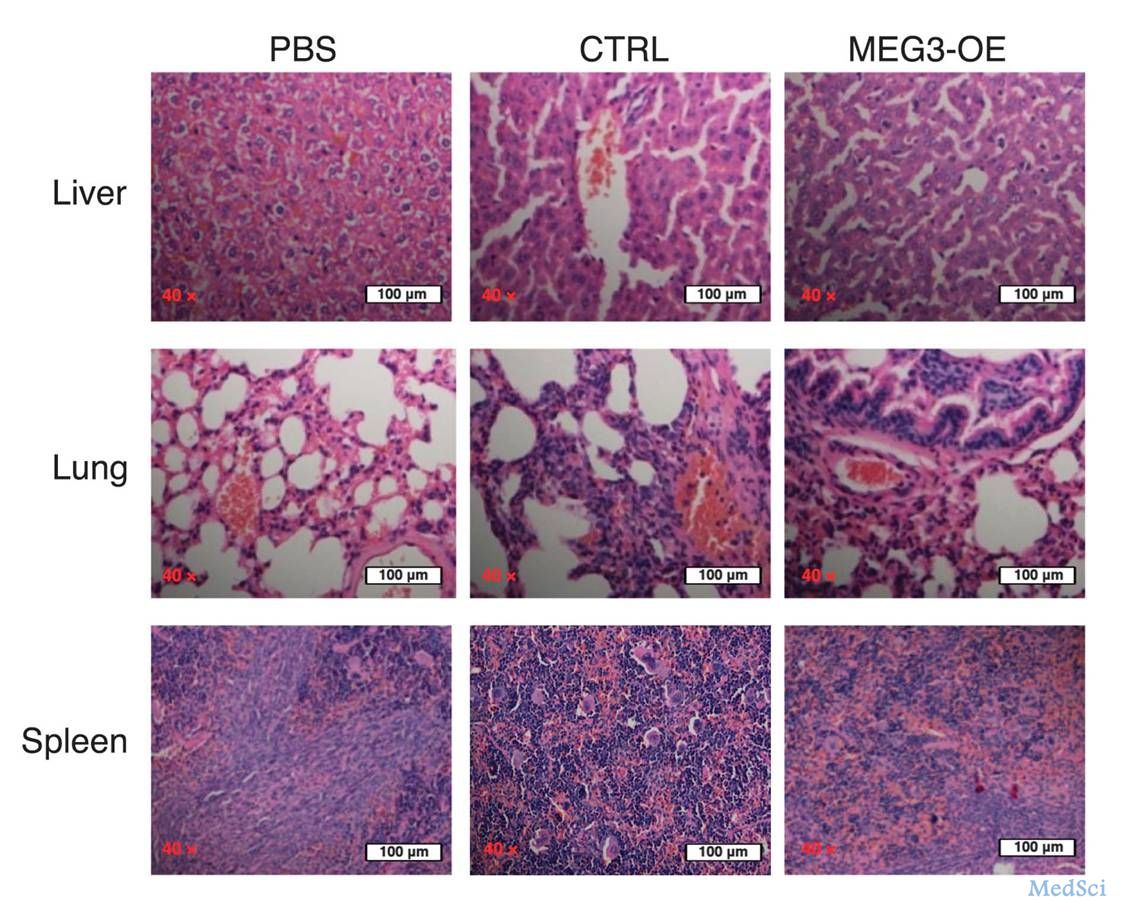







科学家发现WT1-#MEG3#信号通路有望成为治疗#AML#的新靶点,#急性髓系白血病#
96
#WT1#
83
#科学家发现#
73
学习了.谢谢分享
101
#新靶点#
126
#信号通路#
85