JMC:上海药物所南发俊、谢欣课题组合作发现新型抗溃疡性结肠炎候选药物
2022-02-28 细胞 细胞
GPR84是一种促炎型脂肪酸受体,可在炎性刺激下高表达而放大机体的免疫反应,被认为与多种炎症或纤维化疾病的发生发展相关,如炎症性肠病、肺纤维化、肝纤维化等。
2022年2月23日,中国科学院上海药物研究所南发俊课题组、谢欣课题组在Journal of Medicinal Chemistry上发表了题为“Phosphodiesters as GPR84 Antagonists for the Treatment of Ulcerative Colitis”的文章,报道了一种全新骨架的G蛋白偶联受体84(GPR84)选择性拮抗剂,口服可有效缓解炎症性肠病模型小鼠的肠炎症状,疗效优于临床一线药物美沙拉嗪(Mesalazine)。
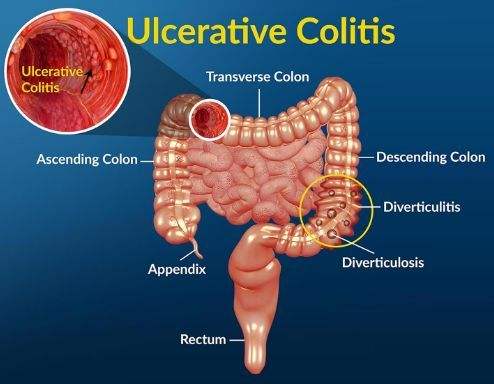
GPR84是一种促炎型脂肪酸受体,可在炎性刺激下高表达而放大机体的免疫反应,被认为与多种炎症或纤维化疾病的发生发展相关,如炎症性肠病、肺纤维化、肝纤维化等。炎症性肠病是一类肠道炎症性疾病,主要包括溃疡性结肠炎(UC)和克罗恩病(CD),其病因不明,反复发作,需终身治疗。目前临床主要根据患者病情分别给予抗菌药、抗炎药或免疫抑制剂等来减缓病情发展,但疾病的反复发作极大降低患者的生存质量。因此,发现治疗炎症性肠病的新靶点及其靶向药物有助于解决未被满足的临床需求。
研究团队与上海市第十人民医院刘占举教授团队合作,采集并分析了炎症性肠病病人的肠粘膜组织样本,发现GPR84表达量在活动期UC病人的样本中明显增加,且增加程度与病情进展显著相关。而敲除GPR84的小鼠在DSS诱导的肠炎中症状显著减轻,证实了GPR84是治疗炎症性肠病的新靶点(Acta Pharmacol.Sin. 2021, doi: 10.1038/s41401-021-00825-y)。
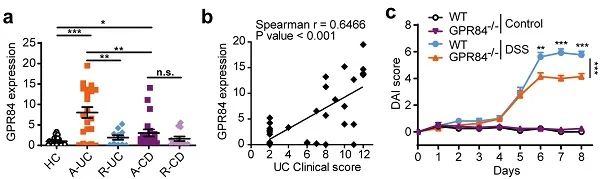
图1. (a) 肠炎病人肠道组织中GPR84表达情况;(b) UC病人中GPR84表达与临床评分间的相关性;(c) GPR84敲除缓解DSS诱导的小鼠肠炎。
在GPR84靶向药物的发现方面,研究团队建立了基于GPR84钙流信号的高通量筛选体系,对国家化合物样品库WNN系列的160,000个化合物开展了大规模随机筛选,发现一个GPR84激动剂ZQ-16(J. Pharmacol. Exp. Ther. 2016, 357, 337-344)和一个全新结构的GPR84拮抗剂CLH536。研究团队对ZQ-16进行了结构优化,发现了迄今为止活性最强的激动剂LY-237(ACS Med. Chem. Lett. 2016, 7, 579-583),受到国际同行关注,并因此受邀就GPR84的相关研究进展撰写综述(J. Med. Chem. 2020, 63, 15399-15409)。研究团队也对CLH536开展了系统的构效关系研究,获得了一系列高活性、高选择性的GPR84拮抗剂。其中,代表性化合物33不仅具有较好的口服吸收和安全性,而且能靶向肠道分布,在口服25 mg/kg起便对葡聚糖硫酸钠(DSS)诱导的小鼠炎症性肠病有显著的缓解作用,中高剂量组(50、100 mg/kg)的疗效优于临床一线药物美沙拉嗪(200 mg/kg)。该化合物正作为抗溃疡性结肠炎候选药物进行临床前开发。
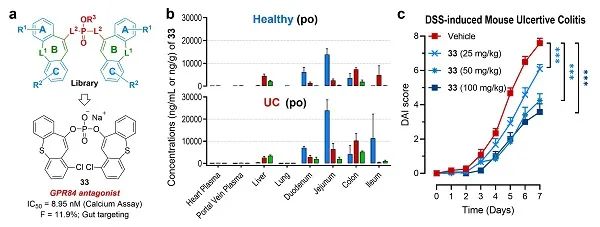
图2. (a) 结构优化策略与化合物33的发现;(b) 33在健康小鼠与UC小鼠中均靶向肠道分布;(c) 33剂量依赖性地缓解DSS诱导的小鼠肠炎。
上海药物所南发俊研究员与谢欣研究员为本研究的共同通讯作者,上海药物所副研究员陈林海、助理研究员张庆和博士毕业生肖瑜峰为共同第一作者。本工作得到了国家自然科学基金委、科技部、中国科学院、上海市科委等项目的资助。
目前该项目已与博骥源(上海)生物医药有限公司达成合作协议,实现了成果转化,并将于近期申报临床。
(供稿部门:南发俊课题组、谢欣课题组、科研与新药推进处)
全文链接:
https://doi.org/10.1021/acs.jmedchem.1c01813
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#候选药物#
103
#溃疡性#
65
学习了
101
#上海药物所#
97