Nat Med:科研人员发现新免疫抑制细胞影响抗肿瘤免疫应答
2018-10-12 李松 新华社
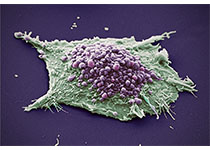
中外科研人员最近研究发现了一种新的免疫抑制细胞会影响抗肿瘤免疫应答,从而影响部分肿瘤患者免疫治疗的效果。这一研究成果已在国际权威学术期刊《自然·医学》在线发表。
据新桥医院肿瘤科朱波教授介绍,近年来,以PD-1/PD-L1抗体为代表的肿瘤免疫治疗取得重大突破,并成为临床肿瘤治疗重要手段之一。但在临床实践中,PD-1/PD-L1抗体治疗肿瘤的有效率仅在20%—30%之间,这除了因为肿瘤细胞可以不断演变逃避免疫识别之外,肿瘤患者体内还可以产生多种具有免疫抑制作用的细胞,如髓系来源抑制细胞等,影响免疫治疗效果。
科学家一直试图探索发现肿瘤患者体内其他的免疫抑制细胞。近期,朱波教授团队联合中外科研机构,在荷瘤小鼠脾脏、肝脏和外周血以及肿瘤患者的外周血中发现了一种新的红系前体细胞来源的免疫抑制细胞,会通过产生活性氧(ROS)抑制CD8+T细胞介导的免疫应答,导致肿瘤患者抗病毒/细菌以及抗肿瘤免疫应答功能的下降。
据了解,正常红系前体细胞本该分化成正常红细胞,但朱波教授团队发现的这种细胞,不但不能正常分化,还产生了极强的免疫抑制能力,使正常的免疫细胞不能有效杀灭肿瘤细胞及清除入侵体内的病原体。该研究为进一步认识肿瘤免疫抑制机制,提高肿瘤患者免疫治疗疗效提供了新思路。
原始出处:
LintaoZhao,RanHe, Haixia,et.al. LongLate-stage tumors induce anemia and immunosuppressive extramedullary erythroid progenitor cells. Nature Medicine
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#科研人员#
86
#Nat#
80
#免疫应答#
80
#Med#
80
了解一下谢谢
88
不错的文章值得拥有,
77