Ann Rheum Dis:系统性硬化症患者的进展性间质性肺病
2020-10-15 xiangting MedSci原创
SSc-ILD存在异质性,并且病程多变,因此对所有患者进行密切随访非常重要。在FVC下降之前就开始治疗的新观念可以避免不可逆的器官损害。
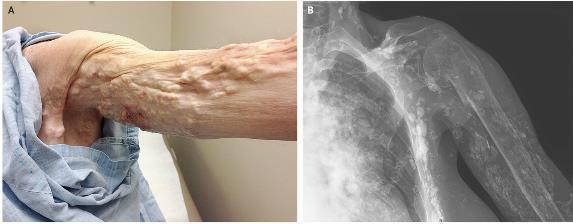
系统性硬化症(SSc)是以局限性或弥漫性皮肤变硬、增厚,同时可伴有肺脏、心脏、肾脏、消化道等内脏器官损伤为特征的少见结缔组织疾病,肺部表现为间质性肺病(ILD),ILD是SSc患者死亡的主要原因,SSc-ILD预后差,死亡率高。这项研究使用欧洲硬皮病试验与研究(EUSTAR)数据库中的数据,确定了SSc-ILD患者出现进展性间质性肺病(ILD)的总体病程、进展模式和危险因素。
EUSTAR数据库对符合条件的SSc-ILD患者进行了登记,在基线和12±3个月后测量用力肺活量(FVC)。对多次测量FVC的患者评估长期进展性ILD和进展模式。使用多因素混合效应模型分析ILD进展的潜在预测因素。
共纳入826例SSc-ILD患者。在12±3个月内,219例患者(27%)表现为进展性ILD:FVC中度下降(降低5%-10%)或显著下降(降低>10%)。平均5年的随访期内,共有535例患者(65%)进行了多次FVC测量。每12个月的周期内有23%-27%的SSc-ILD患者表现为进展性ILD,但只有少数患者呈连续性进展。大多数进展性ILD患者(58%)肺功能下降缓慢,其稳定/改善时间多于下降,而只有8%的患者FVC持续快速下降。178例患者(33%)FVC没有下降。5年内FVC下降的最强预测因素是男性、改良Rodnan皮肤评分高和反流/吞咽困难症状。
SSc-ILD存在异质性,并且病程多变,因此对所有患者进行密切随访非常重要。在FVC下降之前就开始治疗的新观念可以避免不可逆的器官损害。
原始出处:
Anna-Maria Hoffmann-Vold. Progressive interstitial lung disease in patients with systemic sclerosis-associated interstitial lung disease in the EUSTAR database. Ann Rheum Dis. October 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#间质性#
67
#系统性#
110
#硬化症#
80
#Dis#
69
学习了
123
#肺病#
72
#系统性硬化#
105