JCO:奥希替尼进军EGFR突变型晚期NSCLC一线治疗
2017-08-29 佚名 肿瘤资讯
既往AURA系列研究已经显示,在EGFR-TKI耐药后T790M阳性的患者中,奥希替尼疗效显着,对比含铂双药化疗,可以显着延长PFS。目前,奥希替尼已经获批用于EGFR TKI耐药后T790M阳性的患者。在AURA I期研究中,同时入组了部分初治的患者,探索奥希替尼不同剂量组的疗效和安全性,近日,研究结果在《临床肿瘤学》杂志上发表。
既往AURA系列研究已经显示,在EGFR-TKI耐药后T790M阳性的患者中,奥希替尼疗效显着,对比含铂双药化疗,可以显着延长PFS。目前,奥希替尼已经获批用于EGFR TKI耐药后T790M阳性的患者。在AURA I期研究中,同时入组了部分初治的患者,探索奥希替尼不同剂量组的疗效和安全性,近日,研究结果在《临床肿瘤学》杂志上发表。
背景
既往,8大临床研究已经证实,对于EGFR突变型晚期NSCLC,一线EGFR-TKI优于含铂双药化疗,奠定了EGFR-TKI作为EGFR突变型晚期NSCLC一线标准治疗的地位。目前,吉非替尼,厄洛替尼,阿法替尼已经获批用于初治的EGFR突变型晚期NSCLC,汇集多个临床研究的荟萃分析提示,对于初治的晚期NSCLC,一线接受EGFR-TKI治疗的中位PFS为11.0个月,而一线化疗的mPFS仅为5.6个月。尽管患者最初对EGFR-TKI治疗敏感,但最终多数患者会发生继发耐药,其中EGFR T790M突变是最常见的耐药机制,约占60%。
奥希替尼是一个不可逆的EGFR-TKI,选择性作用于EGFR敏感突变和EGFR T790M耐药突变。既往奥希替尼的AURA系列研究已经显示,在EGFR-TKI耐药后T790M阳性的患者中,奥希替尼的疗效显着,ORR为62-70% ,PFS为9.9-12.3个月;在奥希替尼与化疗头对头比较的AURA3研究中,奥希替尼显着优于含铂双药化疗,ORR分别为71% vs. 31%,mPFS分别为10.1m vs. 4.4m。基于上述阳性结果,奥希替尼获批用于EGFR-TKI耐药后T790M阳性的NSCLC。
在临床前研究中,奥希替尼不仅可以抑制EGFR-TKI耐药的细胞株,对于EGFR-TKI敏感突变的细胞株PC9(EGFR exon19del),也显示出较一代TKI吉非替尼更强的活性,此外在临床前模型中发现,EGFR T790M不是奥希替尼的耐药机制。以上证据提示,奥希替尼用于初治的EGFR突变患者,也是非常有效的,可能可以延缓耐药的发生。既往已经报道了AURA I期剂量递增和扩展研究中,奥希替尼用于EGFR-TKI耐药患者的疗效。在AURA研究中,同时还纳入了两个初治患者队列,在此报道奥希替尼用于EGFR突变型晚期NSCLC一线治疗的疗效和安全性。
方法
研究入组了组织学或细胞学确诊的局部晚期或转移性NSCLC,基线时有可测量病灶,经当地或中心实验室确认的组织EGFR突变。允许入组无症状脑转移患者。两个初治患者队列属于剂量探索部分,作为AURA研究的次要研究终点,评估奥希替尼用于初治的EGFR突变型晚期NSCLC的疗效和安全性。入组患者接受奥希替尼80mg或160mg,治疗直至基本进展或达到停药的标准。如果研究者评估患者能从继续治疗中获益,可以在RECIST标准评估为进展后继续用药。
研究疗效终点包括研究者评估的ORR,疗效持续时间(DoR)和PFS。安全性和耐受性采用NCI CTCAE标准评估。此外,在本研究中还进行了一些转化研究探索。分别在用药前和影像学评估进展后收集患者的血浆标本。采用BEAMing数字PCR分析患者基线的血浆EGFR突变状态:EGFR exon19del,L858R和T790M。耐药后的血浆标本采用NGS panel检测。本研究的最后随访日期为2016年11月1日。
结果
共60例初治的EGFR突变型NSCLC接受奥希替尼治疗,80mg/d和160mg/d分别有30例患者,两组患者的基线特征均衡。至数据截止日期,有25例(42%)患者仍在接受治疗,其中80mg/d和160mg/d分别有12例和13例。35例(58%)患者停止治疗,其中24例(40%)是因为疾病进展,5例(8%)为AEs,3例(5%)是患者决定停药,3例(5%)是因为其他原因(临床进展n=1;换用其他抗肿瘤治疗n=2)。
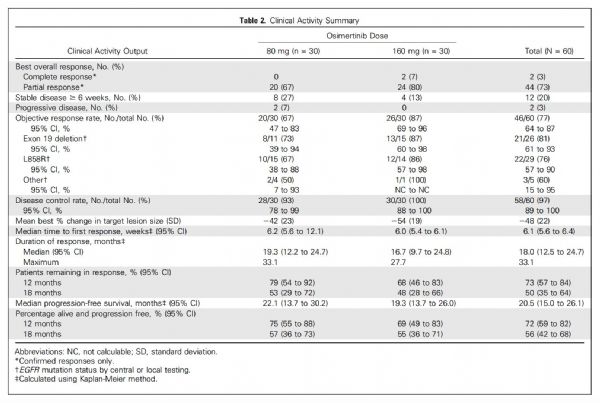
80mg剂量组,160mg剂量组和总体人群中,确认的ORR分别为67% (95% CI, 47%-83%),87% (95% CI, 69%-96%)和77% (95% CI, 64%-87%)。根据EGFR突变类型类分析患者的ORR数据见下表。80mg剂量组,160mg剂量组和总体人群中,DCR分别为93%(95% CI, 78%-99%),100% (95% CI, 88%-100%)和97% (95% CI, 89%-100%)。
表:临床疗效数据汇总
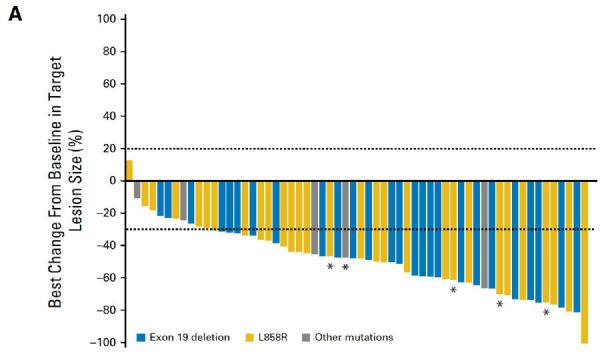
总体人群中,靶病灶最佳缩小比例的平均值为-48%(SD22%),见下图1A。
图A. 患者的疗效瀑布图
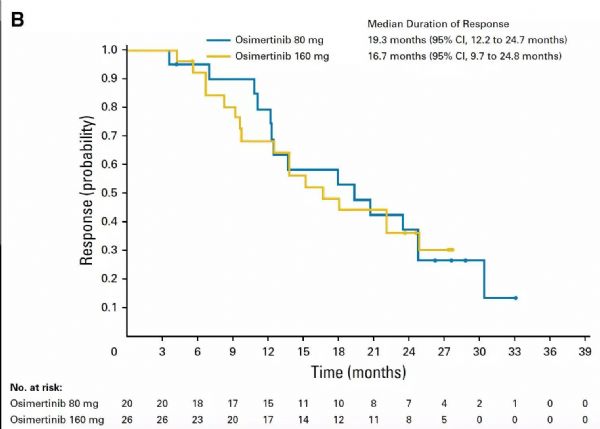
80mg剂量组,160mg剂量组和总体人群中,中位DOR分别为19.3个月(95% CI, 12.3 -24.7),16.7个月(95% CI, 9.7-24.8) 和18.0个月 (95% CI, 12.5-24.7)。80mg剂量组和160mg剂量组患者中,报道的最长的DOR分别为33.1个月和27.7个月。
图B. 奥希替尼不同剂量组患者的疗效持续时间
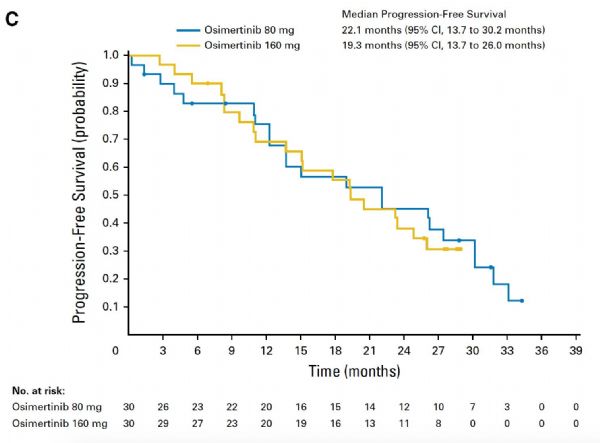
至数据截止日期,42例(70%)患者为RECIST标准评估进展或死亡。80mg剂量组,160mg剂量组和总体人群中,奥希替尼治疗的中位PFS分别为22.1个月(95% CI, 13.7-30.2),19.3个月(95% CI, 13.7-26.0)和 20.5个月(95% CI, 15.0-26.1) 。
图C. 奥希替尼不同剂量组患者的PFS
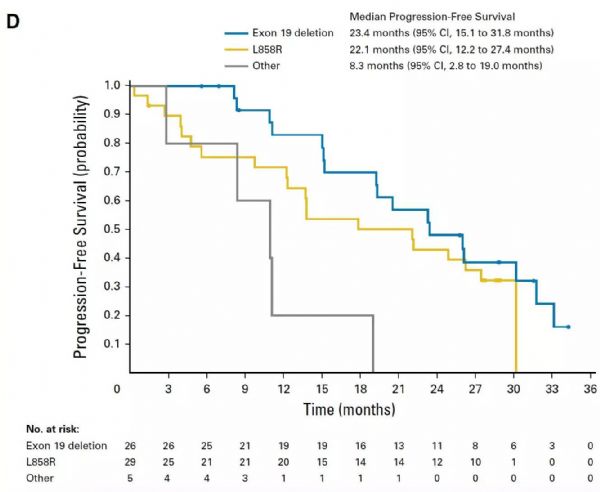
总体人群中,EGFR exon19del,L858R和其他突变患者的中位PFS分别为23.4个月(95% CI, 15.1- 31.8) ,22.1个月(95% CI, 12.2-27.4)和8.3个月 (95% CI, 2.8-19.0)。
图D. EGFR不同突变类型患者接受奥希替尼治疗的PFS
60例患者中,37例(62%)患者在RECIST标准评估为PD后继续接受奥希替尼治疗,中位治疗时间为4.9个月。
血浆分析:
以中心实验室组织标本检测的EGFR突变类型作为参照,采用血浆BEAMing法检测,在T790M和EGFR常见突变的检测时,显示出很好的敏感性。在研究入组时,5例(8%)患者为组织检测确认的原发T790M突变NSCLC,其中4例患者血浆T790M阳性;血浆检测还发现了另外2例T790M阳性的患者(组织未在中心实验室进行检测)。所有血浆检测T790M阳性的7例患者,均伴随L858R突变,其中6例患者治疗的疗效为PR,DOR为6.9-27.7个月。
奥希替尼耐药机制分析:
在数据截止日期,42例(70%)患者为RECIST标准评估为PD,其中38例(91%)患者收集了进展后的血浆标本可以进行NGS分析。其中19例(50%)患者血浆中未检测到ctDNA,其余19例患者可检测到ctDNA。对比两组患者,进展时血浆中有ctDNA患者的mTTP为13.1个月,而血浆中无ctDNA的患者,mTTP为19.6个月。进一步分析19例血浆中有ctDNA的患者,其中9例检测到已知的耐药突变:如既往已经报道过的奥希替尼二线治疗的耐药机制,如MET,EGFR和KRAS扩增,PIK3CA和KRAS突变;2例患者检测到C797S突变,其中1例为de novo T790M突变的患者,1例未合并T790M突变;1例患者检测到MEK1 G128V突变伴EGFR C797S突变。2例患者还检测到其他的激酶突变,HER2 exon20ins,JAK2 V617F。所有的血浆标本中均为发现T790M耐药突变。
结论
本研究是第一次报道奥希替尼用于EGFR突变型晚期NSCLC一线治疗,奥希替尼80mg剂量组的中位PFS为22.1个月,ORR为67%,远远超过既往一代TKI吉非替尼和厄洛替尼用于一些治疗的中位PFS,8.4-13.1个月。以上数据提示,奥希替尼用于EGFR突变型晚期NSCLC一线治疗可以显着延长PFS。
原始出处:
Suresh S. Ramalingam, James C.-H. Yang, Chee Khoon Lee.et al.Osimertinib As First-Line Treatment of EGFR Mutation–Positive Advanced Non–Small-Cell Lung Cancer .Journal of Clinical Oncology
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCO#
59
#突变型#
63
学习了.谢谢分享
96
#晚期NSCLC#
74
#GFR#
61
好文.值得点赞!认真学习了.把经验应用于实践.为患者解除病痛.
95
学习了谢谢作者分享!
84