他汀类药物已被广泛用于降低胆固醇水平和心血管风险。此外,有研究表明他汀类药物可能会降低感染性疾病的风险和感染相关的死亡。然而,他汀类药物的使用与活动性结核(TB)病之间的关系仍不清楚。近日,胸部疾病领域权威杂志Chest杂志上针对这一问题发表了一篇研究文章。
研究人员采用台湾地区健康保险研究数据库进行了一项全国性的基于人群的研究。在2000年-2013年期间,服用他汀类药物且没有原发性结核病的患者被纳入研究。研究人员收集了102424名他汀类药物使用者的数据和202718名年龄、性别和招募日期匹配的对照者的数据,并进行了分析。这两个队列的受试者被随访至2013年12月31日,观察TB疾病的发生。研究人员采用台北荣民总医院索赔数据库对诊断为结核病的患者进行了验证。
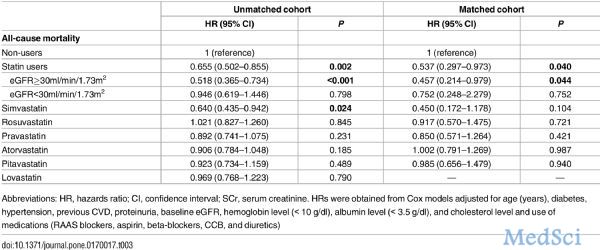
他汀类药物和配对队列分别进行了571568和1027385人次每年的观察。在305142名受试者中,有1264名(0.41%)受试者患上了结核病。研究证实了对结核病诊断的准确性(敏感性为96.3%),具有良好的一致性(κ=1)。多因素分析显示他汀类药物的队列中的患者发生结核病的风险降低(风险比[HR]为0.53,95%可信区间[CI]为0.47-0.61;P<0.001)。与对照组相比,使用他汀类药物与结核病的发生风险呈剂量-反应关系(<180累积限定每日剂量[cDDDs]:HR为1.06,95%CI为0.91-1.24,P=0.477;180-365cDDDs:HR为0.57,95%CI为0.45-0.72,P<0.001;>365cDDDs:HR为0.27,95%CI为0.22-0.33,P<0.001)。
由此可见,他汀类药物可降低结核病的发生风险。
原始出处:
Vincent Yi-Fong Su,et al. Statin Use is Associated with a Lower Risk of Tuberculosis.Chest. 2017. http://journal.publications.chestnet.org/article.aspx?articleid=2627078
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Chest#
52
#EST#
34
#他汀类药#
31
学习了,谢谢分享
83
学习了,感谢分享/。
79
#结核#
34
他汀类药物可降低结核病的发生风险。
68
他汀类降低结核病的发生风险,学习。
67
学习了,谢谢
53
回顾性分析不科学啊,就这样就说明有相管性,患者随访期间有没有服用其它药物呢?
35