World J Urol:根治性膀胱切除术pentafecta的多中心外部验证
2021-07-24 AlexYang MedSci原创
每年全世界有270万人诊断为膀胱癌或因膀胱癌(BCa)而治疗。对于没有转移证据的局部晚期肌层浸润性膀胱癌(MIBC),新辅助铂类全身治疗和根治性膀胱切除术(RC)以及广泛的双侧盆腔淋巴结清扫术(PLN
每年全世界有270万人诊断为膀胱癌或因膀胱癌(BCa)而治疗。对于没有转移证据的局部晚期肌层浸润性膀胱癌(MIBC),新辅助铂类全身治疗和根治性膀胱切除术(RC)以及广泛的双侧盆腔淋巴结清扫术(PLND)是推荐的一线治愈性治疗。然而,这种手术在技术上要求很高,并发症约为25%,死亡率为1-2%,且而不考虑手术方法。包括机器人辅助在内技术的开发减少了围手术期和死亡率。

近期,有研究人员对RC-pentafecta进行了外部验证。

在2014年1月至2019年12月期间,研究人员对6个泌尿外科中心内接受RARC与ICUD的104名连续患者进行了回顾性分析。同时表现出软组织手术边缘(STSMs)阴性、淋巴结(LN)产量≥16、无重大(Clavien-Dindo III-V级)术后90天并发症、无UD相关长期后遗症、无12个月临床复发的患者认为达到了RC-pentafecta。多变量逻辑回归模型用来衡量达到RC-pentafecta的预测因素。研究人员还分析了RC-pentafecta对生存的影响以及对手术经验的影响。
自2014年以来,研究共纳入了104名完成了至少12个月随访的患者。在平均18个月的随访中,分别有56%、96%、85%、81%和91%的患者观察到LN产量≥16,STSMs阴性,90天内无主要并发症,以及≤12个月内无UD相关手术后遗症和临床复发,因此RC-pentafecta比例为39.4%。多变量分析显示,年龄是实现pentafecta的独立预测因素(几率[OR],0.96;95%置信区间[CI],0.90. 0.99;P=0.04)。外科医生的经验对标准的验证有影响。
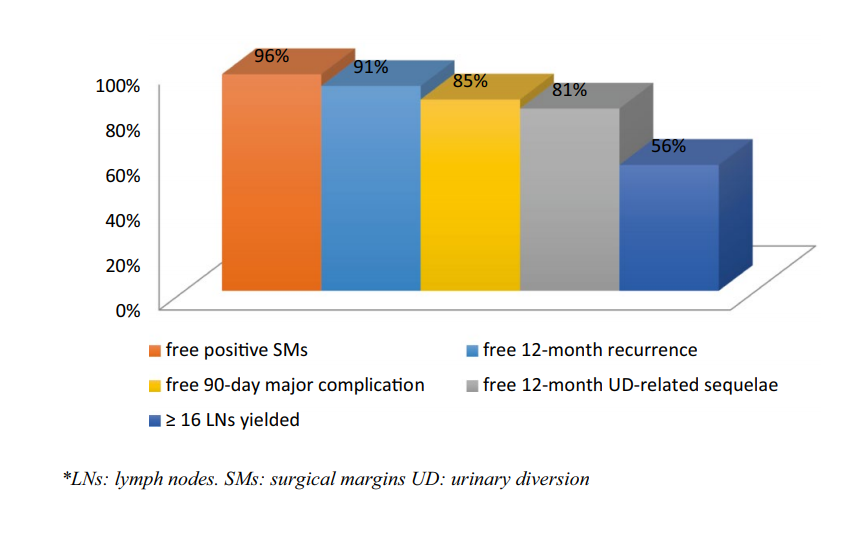
RC-pentafecta标准的百分比
综上所述,RC-pentafecta是可重复的,可以从外部用于RARC与ICUD后的结果评估。因此,RC-pentafecta可以成为评估手术成功及其对不同结果影响的有用工具。
原始出处:
P Baron, Z Khene, F Lannes et al. Multicenter external validation of the radical cystectomy pentafecta in a European cohort of patients undergoing robot-assisted radical cystectomy with intracorporeal urinary diversion for bladder cancer. World J Urol. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#根治性膀胱切除术#
147
#多中心#
66
#PE#
74
#CTA#
79
#切除术#
67
#膀胱切除术#
94
#根治#
77
非常受用
80
非常受用
91
非常受用
93