Gastroenterology:食管黏膜阻抗或为新选择
2015-02-10 王姗编译 中国医学论坛报
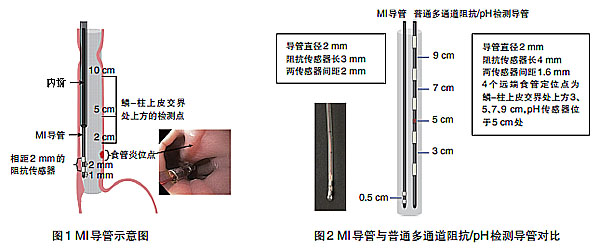
■研究简介 一项美国前瞻性研究表明,食管黏膜阻抗(MI)检测(图1~2)在胃食管反流病(GERD)诊断方面的特异性和阳性预测值均高于无线pH值监测。论文发表于《胃肠病学》杂志[Gastroenterology2015,148(2):334]2月刊。 研究共纳入61例糜烂性食管炎患者、81例非糜烂性但pH异常的GERD患者、93例无GERD者、18例贲门失弛缓症患者及15例嗜

■研究简介
一项美国前瞻性研究表明,食管黏膜阻抗(MI)检测(图1~2)在胃食管反流病(GERD)诊断方面的特异性和阳性预测值均高于无线pH值监测。论文发表于《胃肠病学》杂志[Gastroenterology2015,148(2):334]2月刊。
研究共纳入61例糜烂性食管炎患者、81例非糜烂性但pH异常的GERD患者、93例无GERD者、18例贲门失弛缓症患者及15例嗜酸性食管炎患者。对所有受试者均行MI检测,检测部位为食管鳞-柱状上皮交界上方2cm、5cm及10cm处,抑酸治疗前后均进行MI检测,并将结果与无线pH值监测相比较。
结果为,GERD(糜烂性食管炎或非糜烂性但pH异常)患者或嗜酸性食管炎患者的MI值明显低于无GERD者或贲门失弛缓症患者(P<0.001)。GERD患者的MI模式与无GERD者或嗜酸性食管炎患者不同,在接近食管鳞-柱状上皮交界处其MI值较低,沿食管纵轴向上MI值升高;且在给予抑酸治疗后此种模式可恢复正常。在分辨食管炎患者方面,此种MI模式与无线pH值监测相比具有更高的特异性(95%对64%)和阳性预测值(96%对40%)。
■同期述评
食管黏膜阻抗:可摒弃长时胃食管反流检测?
虽然上述研究表明,MI检测可将GERD患者从无GERD者中区分出来,但问题是,决定MI的因素是什么?这些因素将左右检测的结果。
MI导管所测量的跨膜阻抗和渗透性受食管黏膜结构改变的影响,因此任何导致食管黏膜完整性改变的物质均可造成MI变化。MI导管可能无法区别非反流相关的食管黏膜结构异常和反流相关的食管黏膜改变。
另一个更为重要的问题是,MI检测是否可以替代现有的胃食管反流检测方法(阻抗+pH检测、24小时pH检测及无线pH胶囊检测)。尽管MI检测简单易行,但未能提供胃食管反流的程度、类型及模式等信息,且不能区分酸性及非酸性的食管黏膜结构改变及反流主要发生于白天还是夜间,也不能确定反流暴露的高度及反流事件和症状之间的相关性,在评价症状改善方面亦具有局限性。
尽管MI检测尚无法替代现有的胃食管反流程度评估检测,但其简易性和结果的直接可用性对繁忙的临床消化科医生极具吸引力。此外,对于无法耐受须经鼻置管24小时的阻抗+pH检测或24小时pH检测的患者,MI检测或为重要的评估工具。
更重要的是,这项技术可很好地区分临床上难以分辨的GERD与功能性烧心的患者,并可对其他食管功能检测进行补充,提供食管黏膜结构完整性的额外信息。
原始出处:
Ates F1, Yuksel ES1, Higginbotham T1, Slaughter JC2, Mabary J3, Kavitt RT1, Garrett CG4, Francis D5, Vaezi MF6.Mucosal Impedance Discriminates GERD From Non-GERD Conditions.Gastroenterology. 2015 Feb;148(2):334-43. doi: 10.1053/j.gastro.2014.10.010. Epub 2014 Oct 16.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GAS#
56
#AST#
51
#Gastroenterol#
63
不错,不错!收藏!
226
还行
167
不错的文章,学习了
188
以阅
146
#食管#
56
#Gastroenterology#
69
#黏膜#
69