Nat Med:Tisagenlecleucel治疗复发性或难治性滤泡性淋巴瘤效果如何?
2021-12-20 MedSci原创 MedSci原创
Tisagenlecleucel对于广泛预处理的复发性/难治性FL患者是安全有效的,包括高危患者。
Tisagenlecleucel是一种自体抗CD19嵌合抗原受体T细胞疗法,在复发性/难治性B细胞淋巴瘤患者中显示出具有临床意义的结果。FDA发布了第一个嵌合抗原受体(CAR)T细胞疗法,授权使用Tisagenlecleucel治疗25岁以下B细胞前体急性淋巴细胞白血病(ALL)的患者,在既往对Tisagenlecleucel治疗复发性/难治性滤泡性淋巴瘤(FL)的初步研究中,71%的患者获得了完全缓解(CR)。

近日,顶级医学期刊Nature Medicine上发表了一篇研究文章,在这项研究中,研究人员报告了对Tisagenlecleucel的ELARA2期多国试验的初步、预先指定的中期分析。该试验在接受两个或多个疗程后复发或需要自体干细胞移植的复发性/难治性FL成人(编号NCT03568461)中进行,其主要终点是CR率(CRR),次要终点包括总反应率(ORR)、反应持续时间、无进展生存期、总生存期、药代动力学和安全性。

截至2021年3月29日,97/98名入组该研究的患者接受了Tisagenlecleucel治疗(中位随访时间为16.59个月;四分位距为13.8-20.21),且达到了该研究的主要终点。在疗效组(n=94)中,CRR为69.1%(95%置信区间为58.8-78.3)和ORR为86.2%(95%置信区间为77.5-92.4)。
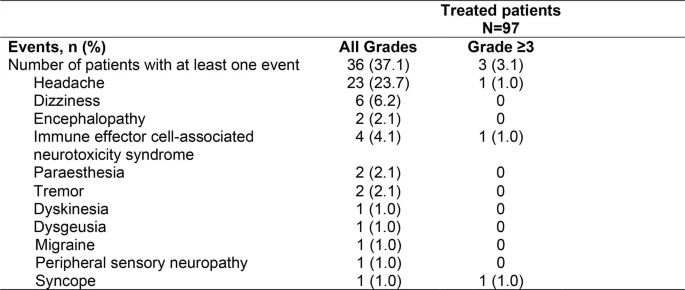
在安全组(n=97)中,输注Tisagenlecleucel的8周内,细胞因子释放综合征的发生率为48.5%(等级≥3,0%),神经系统事件为37.1%(等级≥3,3%)和免疫效应细胞相关神经毒性综合征(ICANS)为4.1%(等级≥3,1%)。没有发生与治疗相关的死亡。
由此可见,Tisagenlecleucel对于广泛预处理的复发性/难治性FL患者是安全有效的,包括高危患者。
原始出处:
Nathan Hale Fowler,et al.Tisagenlecleucel in adult relapsed or refractory follicular lymphoma: the phase 2 ELARA trial.Nature Medicine.2021.https://www.nature.com/articles/s41591-021-01622-0#Abs1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
67
#复发性#
79
#CEL#
69
#滤泡性淋巴瘤#
131
#难治性#
63
#Med#
64