上眼睑时有脓肿 皮肤结核?皮肤着色芽真菌病?
2018-11-14 赵俊英 王增芳 专家会诊中心病例讨论精选
65岁男性,半年前右前额受外伤,其后皮损始终未愈合,波及右上眼睑,时有脓肿。根据皮损的形态、分布,真菌培养,终确诊。究竟是皮肤结核、皮肤着色芽真菌病,还是其他疾病作祟?
65岁男性,半年前右前额受外伤,其后皮损始终未愈合,波及右上眼睑,时有脓肿。根据皮损的形态、分布,真菌培养,终确诊。究竟是皮肤结核、皮肤着色芽真菌病,还是其他疾病作祟?
病历摘要
患者,男,65岁,农民。
主诉:右前额及上眼睑皮疹伴瘙痒半年。
现病史:半年前右前额受外伤,其后皮损始终未愈合,波及右上眼睑,时有脓肿。
家族史:家族中无慢性病及类似病史。
体格检查
一般情况:一般状态可,内科系统检查未见异常。
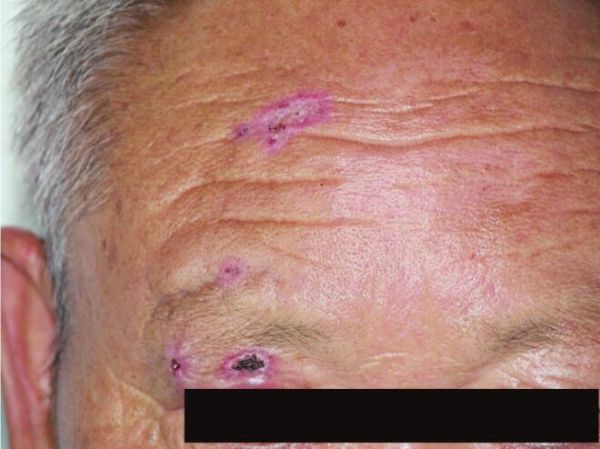
专科情况:右侧前额、右眼睑可见环形红斑,中心结痂,渗出明显(图1-2-5)。
辅助检查
尿糖(+),血糖6.8mmol/L(餐后2小时),血常规:大致正常;真菌镜检(-),真菌培养:孢子丝菌(+)(图1-2-6)。
图1-2-5 右侧前额、右眼睑可见环形红斑,中心结痂,渗出明显
图1-2-6 孢子丝菌
讨论内容
该患者为老年男性,病史半年。皮损表现为右侧前额、右眼睑环形红斑,中心结痂,渗出明显。根据皮损的形态、分布,真菌培养可见孢子丝菌,考虑诊断为“孢子丝菌病”。本病须与以下疾病鉴别:
1.皮肤结核
皮肤结核有多种皮肤损害,疣状皮肤结核易与疣状增生状孢子丝菌病相混淆;寻常性狼疮易与浸润斑块状或溃疡性孢子丝菌病相混淆;瘰疬性皮肤结核的囊肿外观上,颇似本病的囊肿性损害。丘疹状坏死性结核与本病的播散型和痤疮样型容易误诊,主要依靠真菌学检查加以区别。病理活检可鉴别参考。孢子丝菌病典型的改变为三区结构,但有的病例为结核样肉芽肿。此时病理学鉴别则较困难,一般从病理角度观察结核的上皮样细胞较为紧凑成团状,而中央或有或无干酪样坏死。而本病的结核样肉芽肿的上皮样细胞团较为松散,往往在上皮样细胞区中央有少数中性粒细胞。并需注意观察病原体,必要时做PAS染色及抗酸染色。
2.结节病
结节病易与本病的结节状、斑块角化状损害混淆,真菌学检查可资鉴别。组织病理改变与本病的结核样肉芽肿改变混淆。但结节病的上皮样细胞团被结缔组织包绕,有时在朗格汉斯细胞内可见绍曼小体和星状小体。这种星状小体与本病的星状体不同,它位于朗格汉斯细胞内,而且星状小体的中央没有孢子,真菌培养可以鉴别。
3.皮肤肿瘤
本病误诊较多的是鳞状细胞癌、鲍恩病、基底细胞上皮瘤,其次是小汗腺癌、角化棘皮瘤等。与肿瘤的鉴别主要依靠组织病理学检查。真菌学检查也可以区别。已有本病发生鳞状细胞癌的报告。
4.皮肤着色芽真菌病
着色芽真菌病的发病部位与本病基本相同,也多由外伤致感染暗色丝孢科真菌发病。特征为疣状皮肤结节,逐渐形成乳头瘤样增生,或可破溃形成溃疡、结痂等。其临床表现颇似本病,其病理变化也较难与本病区别,不过着色芽真菌病在HE染色下容易见到厚壁孢子,孢子散在或3~5个群集。孢子壁厚,双层,有轻微皱褶,呈黄褐色,有时在孢子周围组织内有少量黄色物质沉积。有的病例也可见到星状体。真菌培养菌种鉴定可以区别,免疫荧光检测、孢子丝菌素皮肤试验可做参考诊断。
5.皮炎芽生菌
是由皮炎芽生菌所致慢性肉芽肿性化脓性疾病。由呼吸道引起感染,主要侵犯肺,并可播散到皮肤和骨骼等部位。我国罕见本病,国外已有病例报道,主要发生于美国、加拿大等地。其皮损与孢子丝菌病的溃疡性或肉芽增生性损害相似。真菌培养菌种鉴定可以区别。
6.皮炎芽生菌样脓皮病
并非罕见,与本病的固定型溃疡肉芽增生状损害、坏疽性脓皮病样损害相似。病理变化主要为表皮假上皮瘤样增生,并有表皮内中性粒细胞性小脓肿,真皮内以弥散性急性炎症为主,伴有嗜酸性粒细胞浸润。病理检查、真菌培养可以鉴别。
7.晚期梅毒疹
结节状梅毒疹、梅毒树胶肿与本病的结节状、疣状增生状损害容易混淆,但病理检查、血清反应及真菌培养可资鉴别。
8.皮肤利什曼病
皮肤利什曼病特别是发生于面部的结节性损害与本病的结节状损害相似。其病理改变主要为单一核细胞性肉芽肿,在巨噬细胞内见有利什曼原虫,Giemsa染色看得更清楚,真菌培养阴性,可资鉴别。
最终诊断:孢子丝菌病。
治疗经过
口服特比萘芬250mg,每日一次,口服维生素B6 100mg,每日两次,2周后复查皮损较前减轻,后失访。
讨 论
孢子丝菌病(sporotrichosis)是由孢子丝菌感染所致,主要引起皮肤感染,也可引起黏膜、骨骼甚或系统性病变。本病于1898年由美国Shenck首先报道,并分离出病原菌。申克孢子丝菌为侧孢霉双相型真菌,所致孢子丝菌病为人、畜共患慢性感染性疾病。本菌在自然界为腐生寄生菌,广泛存在于柴草、芦苇、粮秸、花卉、苔藓、草炭、朽木、土壤、沼泽泥水等处,在以上物质中均可分离出本菌。传染源是患本病的人或动物,传播媒介主要是被孢子丝菌污染的柴草、腐植和土壤等。传播途径主要是皮肤受到外伤时病原菌乘机植入,少数情况下可通过呼吸道吸入病原菌而致病。
孢子丝菌是腐生菌,可附于土壤、动物、植物或敷料等上,通过损伤的皮肤或黏膜进入人体内,构成异物和抗原。经过一定的潜伏期,局部首先出现化脓性炎症反应,接着出现中性粒细胞浸润或形成小脓肿,继而局部组织细胞增生,引起淋巴细胞、浆细胞、巨噬细胞、上皮样细胞、多核巨细胞反应,局部形成肉芽肿性改变。如果侵入的病原菌数量少、皮肤损伤部位反应适当、机体免疫力强、病原菌被吞噬细胞清除,也有可能在发生孢子丝菌病性“初疮”之后,逐渐形成固定型损害或淋巴管型损害。但当机体的免疫力低下时,病原菌进入人体后可以通过血液循环播散全身而引发播散型或系统型孢子丝菌病。因此,机体免疫力在本病发生中起重要作用。
皮肤固定型孢子丝菌病的典型特征是在初疮出现后,逐渐扩大、加重,形成炎症性斑块或增生性糜烂结痂面,甚或形成溃疡。肉芽组织呈乳头状或颗粒状,表面覆以污秽结痂,痂下有少量血性渗出物。皮肤淋巴管孢子丝菌病的特点是初疮出现后局部逐渐扩大、加重,不久即沿回流淋巴管向近端发展,出现炎症性结节,初为豆粒大小,不红,逐渐增大增多,散在分布,各个结节间有一定间距,几个或十几个,甚或几十个,呈串珠状。结节间淋巴管出现炎症,条索状增粗,质硬,轻压痛,但附近淋巴结肿痛不明显。结节可形成脓肿、溃疡、囊肿等。溃疡的肉芽多呈暗红色、颗粒状、脆而易碎。本型初疮多发生于肢体末端,继发皮损沿淋巴管向近端发展,但很少越过腋下或腹股沟区淋巴结继续向躯干发展。皮肤播散型多由淋巴管型发展而来,易发生于营养不良、免疫力低下、长期应用糖皮质激素或年老体弱的患者;或是病原菌感染后尚未形成明显的初疮,病原菌通过血液循环播散而引起皮肤散在多量损害,可见炎症结节、脓肿、溃疡、炎症性囊肿等。
传统的申克孢子丝菌的诊断主要依靠真菌直接镜检及培养,前者特异性差,阳性率低,且不能鉴定菌种,后者耗时,不能满足科研及临床的需要。虽然荧光抗体和免疫组化技术也提供了一种快速诊断孢子丝菌的方法,但它们在大部分临床实践中不被应用。目前分子生物学技术已应用于病原真菌的种型鉴定和亲缘关系研究,这些技术主要包括任意引物聚合酶链式反应(random amplified polymorphic DNA,RAPD)、限制性片段长度多态性分析(restriction fragment length polymorphism,PCR-RFLP)、单链构象多态性分析(single strand conformation polymorphism analysis of polymerase chain reaction products,PCR-SSCP)、分子探针技术和DNA序列分析等,一些已经被引进至快速鉴定申克孢子丝菌的诊断中。
根据国内报道病例分析,碘化钾仍是治疗本病的首选药物。唑类抗真菌药物治疗本病是有效的。张丽佳等研究应用氟康唑注射、克霉唑乳膏与碘化钾联合治疗,具有疗效佳、疗程短、减少不良反应等优点。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#眼睑#
125
456
124
3
117
2
99
1
113
123
98
#结核#
69
#真菌#
73
#脓肿#
56