2017版NCCN临床实践指南更新的要点解析-直肠癌
2016-11-30 温医一院 李绍堂 全球结直肠医学高峰论坛
2016年11月23日,NCCN在线发布了2017版结肠癌和直肠癌临床实践指南,和2016年V2版对比,出现了很多目前临床热点问题的推荐更新,在结肠癌临床实践指南里加入了有争议的左右半肠癌分子靶向药物推荐方案。最重要的是直肠癌临床实践指南,对临床上具有争议的恶性息肉处理、T3直肠癌治疗方法、mCRC新辅助化疗方案、免疫治疗、转移灶毁损性治疗方法选择等给出了明确的更新推荐。以下是笔者对2017版
来源:全球结直肠医学高峰论坛(微信ID colorectal-surgeons)
作者:温医一院 李绍堂
1.关于恶性息肉局部切除后的处理
恶性息肉(癌细胞浸润穿透黏膜肌层到达黏膜下层pT1)局部切除后病理提示高风险(切缘阳性、淋巴血管侵犯、分化程度差、sm3等情况)患者的后续治疗一直是临床上比较有争议的问题。虽然2016版NCCN指南建议对具有预后不良的组织学特征者(病理提示高风险),即使术后追加了放化疗,也应该考虑行经腹直肠切除术以保证可以行淋巴清扫。但是,2017版指南给出选择性推荐。局部切除术后病理提示高风险患者放化疗以后根据情况可以有3种选择①.CR患者监测随访(新推荐)。②追加经腹直肠切除术。③ FOLFOX/CAPEOX方案辅助化疗(新推荐,图1)。这是NCCN指南首次推荐CR患者观察等待(watch-and-wait),估计这个推荐很快会应用于其它不同分期直肠癌辅助治疗后的CCR患者。
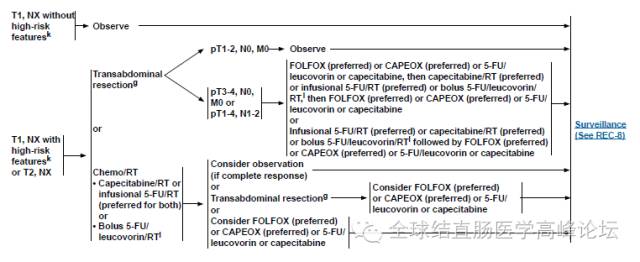
图1
2.关于术前临床评估与术后病理分期不相符情况的处理
虽然直肠癌目前利用ERUS、CT、MRI和PET-CT进行术前评估,评估的准确性有了明显的提高,但是仍然存在20%左右的评估不足和评估过度。由于直肠癌患者往往涉及到放疗,如果评估不足的患者术后追加放疗,术后放疗的患者急慢性毒副反应明显较术前放疗增加。如果评估过度,就存在过度的治疗。2016版NCCN指南对术前评估cT1-2N0M0,术后pT3-4N0M0,均推荐术后放化疗。然而,2017版指南推荐:根据情况可以有3种选择①监测随访(新推荐)②辅助化疗(新推荐)。③辅助放化疗。临床医师可以结合患者情况,可以选择其中一种方案。从这里我们可以看出指南推荐放疗的力度明显下降(无论术前或者术后,图2)。同时,笔者个人认为该条推荐还可以用于术前评估T3的患者,特别是MRF阴性T3患者建议不需要术前新辅助治疗,术后pT3N0M0、CFM阴性、即使术前没有新辅助治疗,建议不需要术后辅助放化疗,只需要监测随访。此外2017版指南删除了“术前接受过辅助治疗的患者,无论术后病理分期情况如何,均因接受术后辅助治疗”的推荐。从这里我们可以理解,术后需不需要辅助治疗,主要根据术后的病理情况,和术前有无接受新辅助治疗无直接关系。
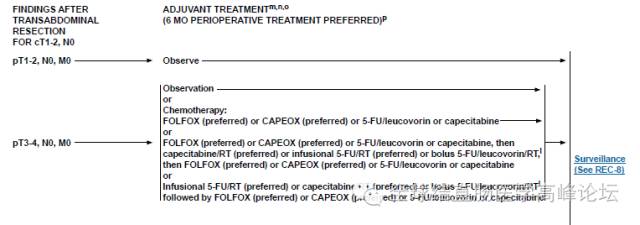
图2
3.关于可切除mCRC新辅助化疗方案2017版NCCN指南将mCRC新辅助化疗方案直接更新为FOLFOX/CAPEOX/FOLFIRI,删除了分子靶向药物的推荐(图3)。我个人不赞同NCCN对于在新辅助化疗中完全删除靶向药物的更新。很显然,为什么不可切除的患者转化治疗可以推荐加分子靶向药物,而可切除患者不推荐,似乎存在矛盾。mCRC患者辅助治疗靶向药物的选择,不应该只根据肿瘤可不可以切除来选择需不需要加靶向药物,主要还要结合肿瘤的生物学行为,疾病的程度。个人建议参考ESMO指南的观点比较合理,一定要从"技术标准"和"预后信息"两个维度来参考决策,对于预后很差(评分4-5分)的技术上"可切除"mCRC,术前新辅助治疗不应该排除靶向药物,赞成陈功教授的观点。
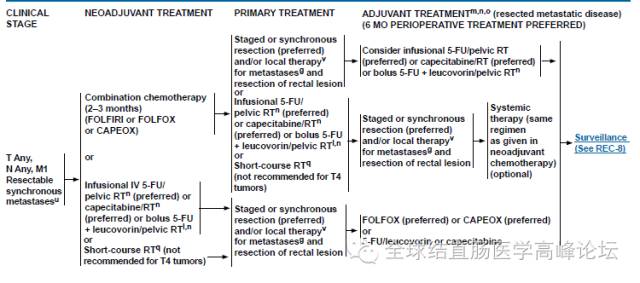
图3
4.免疫治疗方面2017版NCCN指南中首次将免疫检查点抑制剂PD-1单抗Pembrolizumab和Nivolumab推荐单独用于具有dMMR/MSI-H分子表型的,12个月内进行FOLFOX或CAPOX治疗的,不可切除的mCRC的转化治疗或者辅助治疗(图4)。虽然很多学者认为PD-1单抗为正陷于治疗困境中的mCRC带来了突破性进展,它开启了免疫治疗的另一个新思路—基于基因/标志物富集的"精准"免疫治疗。但是,最近医学顶级期刊《柳叶刀》旗下的《TheLancet Oncology》近期报导了Stéphane Champiat和同事的一项新研究。该研究发现,部分肿瘤患者在接受了PD-1/PD-L1单克隆抗体治疗后,癌症的进展加速了,该篇报道引起了广泛的关注和PD-1/PD-L1研究人员的重视。该项研究揭示了一小部分肿瘤患者使用PD-1/ PD-L1抗体后,呈现出疾病高度进展的模式(HPD)。HPD结果与年龄显著相关,HPD患者普遍年龄较大,尤其是65岁以上较多。数据显示,19%65岁以上的患者有HPD,但只有4%的64岁以下患者有HPD。这项发现引起了人们对老年患者(> 65岁)治疗的关注。笔者对于PD-1 / PD-L1抗体单一治疗mCRC持谨慎乐观态度。希望后续进一步研究揭示这种现象的原因。
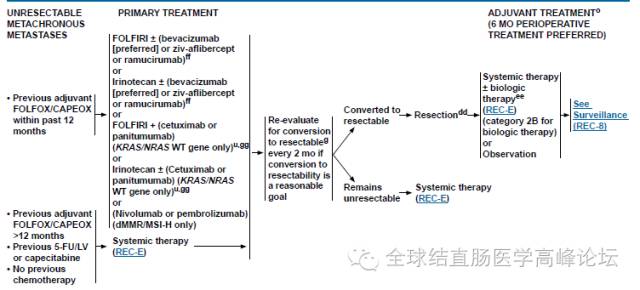
图4
5. 关于转移灶毁损性治疗方法选择的问题2017版NCCN指南明确提出转移灶手术切除优于其他毁损性治疗方法如射频消融、立体定位放射治疗(SBRT)等等。但是射频消融, SBRT可以作为肝肺寡转移灶治疗备选方法。
6.关于治疗后随访计划
2017版NCCN指南首次提出根据不同的分期采取不同的随访计划。对于I期患者推荐结肠检查随访就可以了。II、III期患者术后2年内的胸腹部CT检查频率从原来推荐的3-6月/次降低到6-12月/次(图5)。随访计划的调整,更显示肿瘤防治的个体化。从这一点我们可以看到全球医疗正转入“价值导向”的模式。
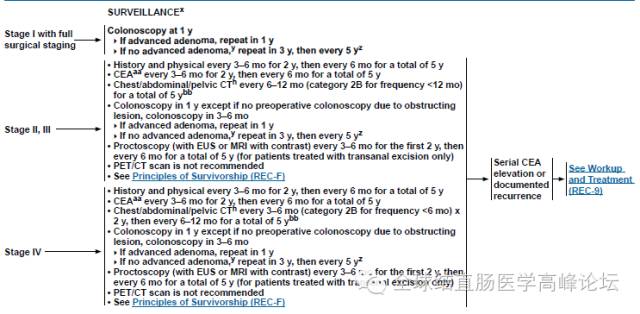
图5
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#指南更新#
55
#解析#
56
.^.↖一.☆\↘
105
赞一下,学习了!
102
#实践指南#
55
#NCCN#
0
#临床实践#
94
#临床实践指南#
55
了解了解!
124
很好,不错的指南资料,值得拥有值得收藏,值得探究。给自己学习探究提供方便。点个赞!
89