PBMB:单个细胞如何发育演变成脊椎动物大型机体?
2016-09-04 佚名 生物谷
图片摘自:www.nature.com近日,发表在国际杂志Progress in Biophysics & Molecular Biology上的一项研究报告中,来自曼荷莲学院等机构的研究人员提出了一种新的理论,解释了为何在机体发育期间复杂的脊椎动物机体来源于单细胞以及随着时间这些系统进化的机制,其中就包括骨骼、肌肉、神经和心血管系统等,这种理论称之为胚胎几何学,其是20年来科学家们工作的
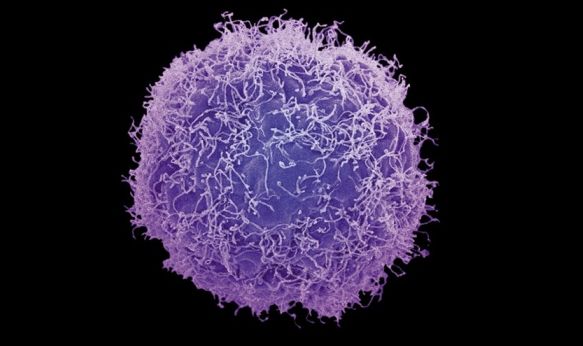
图片摘自:www.nature.com
近日,发表在国际杂志Progress in Biophysics & Molecular Biology上的一项研究报告中,来自曼荷莲学院等机构的研究人员提出了一种新的理论,解释了为何在机体发育期间复杂的脊椎动物机体来源于单细胞以及随着时间这些系统进化的机制,其中就包括骨骼、肌肉、神经和心血管系统等,这种理论称之为胚胎几何学,其是20年来科学家们工作的一项重大突破;而且这种新理论或许也可以应用于不同的脊椎动物器官系统中。
新达尔文学说指出,随着时间延续,主要的进化改变往往是随机的选择以及意外的遗传突变所致,然而有些研究者认为这种理论并不能完全从根本上说明不同的生命形式以及其机体的复杂性,尤其是在脊椎动物比如人类中观察的机体复杂性。文章中研究者提出的这种胚胎几何学理论着眼于观察动物的复杂性以及脊椎动物的机体复杂性,尤其是机械力和相关几何学法则的产物,而并不是单一的随机遗传突变所引发的后果。
研究者Stephen Jay Gould说道,我们希望这种胚胎几何学的理论能够激起我们后期更加深入的探索和研究;长期以来解剖学家假设,动物机体的复杂性或源于胚胎发育阶段,但尽管我们对所有主要类型动物的胚胎发育阶段进行了详细地描述,个体发育阶段有机体进化的复杂性以及其基因表达目前仍然是个谜题。
提出胚胎几何学的研究者表示,脊椎动物的胚胎起源于囊胚的机械变形,当受精卵分裂时就会形成囊胚细胞,随着这些细胞增殖,囊胚球状细胞就会增加体积和表面,并且改变其几何学特性,这种理论认为,囊胚可以维持最开始受精卵三分裂时产生的最原始的八个细胞的几何学特性,而这或许就可以帮助确定脊椎动物机体的三轴特性。
这项研究中,研究者提出了24个梗概图(蓝图),这些蓝图揭示了机体肌肉骨骼、心血管系统、神经系统以及生殖系统如何通过几何学模式的机械变形所形成,而且其或许也可以帮助解释在进化过程以及个体胚胎发育阶段脊椎动物的机体如何基于单细胞而发育产生,与此同时研究者还完成了对花及果蝇起源奥秘的解释。
原始出处
David B. Edelmana, , Mark McMenaminb, , Peter Sheesleyc, , Stuart Pivard.Origin of the vertebrate body plan via mechanically biased conservation of regular geometrical patterns in the structure of the blastula.PBMB.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#演变#
49
#发育#
31
#脊椎#
26
阅读了。
33