J Nucl Med:用于监测靶向免疫制剂治疗的PET放射性示踪器
2017-04-09 MedSci MedSci原创
在The Journal of Nuclear Medicine四月刊发表的一篇文章中,加利福尼亚斯坦福大学的研究人员提供了一个评估新型正电子发射断层扫描(PET)放射性示踪剂的模型,该放射性示踪剂可以准确识别癌细胞中阻止免疫系统攻击癌症的分子。
在The Journal of Nuclear Medicine四月刊发表的一篇文章中,加利福尼亚斯坦福大学的研究人员提供了一个评估新型正电子发射断层扫描(PET)放射性示踪剂的模型,该放射性示踪剂可以准确识别癌细胞中阻止免疫系统攻击癌症的分子。
免疫检查点抑制剂,是目前比较有前景的一种癌症治疗方法。然而,缺乏评估免疫检查点表达的成像工具一直是预测和监测对临床检查点封锁的反应的主要障碍。
"因为癌症免疫疗法正在扩大,所以需要通过分子成像优化个体患者的治疗方法。"斯坦福大学医学博士Sam Gambhir解释说。"这项研究通过动物模型验证了几种新开发的工程化PET示踪剂,这些示踪剂可以辅助免疫系统成像,并用于监测检查点抑制剂治疗。"
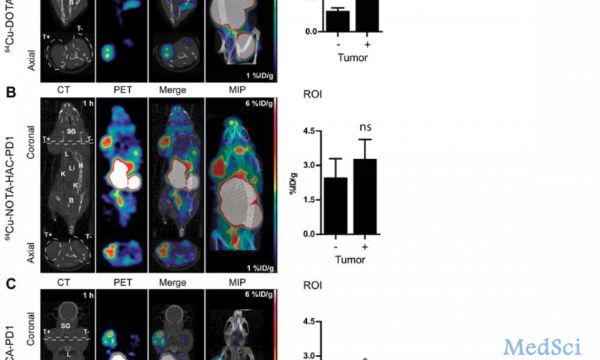
该研究评估了实际免疫PET放射性示踪器设计修改及其对人PD-L1免疫检查点成像的影响。研究人员力求优化工程设计参数,包括螯合物,糖基化和放射性金属,以开发非侵入性分子成像工具,最终实现对临床检查点封锁的监测。
Gambhir指出,"这项研究最终将允许动物模型中的最佳示踪剂运用到人体影像中。一种有效的免疫PET放射性示踪剂将帮助患者选择最佳免疫检查点抑制剂治疗药物以抗击癌症。"
分子成像在免疫治疗和个性化医学中发挥越来越重要的作用。展望未来,Gambhir希望"在对患者进行免疫疗法时能更多的使用PET / CT或PET / MR进行辅助诊断。" 他补充说:"这项相关研究还将有助于我们开发其他成像方法来了解免疫系统的作用。"
原文出处:
Aaron T. Mayer,et. al. Practical ImmunoPET radiotracer design considerations for human immune checkpoint imaging. Journal of Nuclear Medicine (2017).
此文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PE#
76
#PET#
78
#Med#
76