Oncogene:前列腺癌中FRMD6具有抑制肿瘤的功能
2020-12-16 AlexYang MedSci原创
现有的前列腺癌(PC)预后工具不是最优的,但可能通过更好地了解驱动肿瘤侵袭性的基因来改善。
现有的前列腺癌(PC)预后工具不是最优的,但可能通过更好地了解驱动肿瘤侵袭性的基因来改善。
最近,有研究人员鉴定了FRMD6(包含FERM结构与的蛋白6)是PC中一个异常超甲基化和显著下调的基因。在两个大型PC患者队列中,FRMD6的低表达与术后生化复发相关。在PC细胞系的过表达和CRISPR/Cas9敲除实验中,FRMD6能够抑制生存力、增殖、细胞周期进展、克隆形成、3D球体生长和肿瘤异种移植生长。转录组、蛋白质组和磷酸蛋白质组分析显示,FRMD6敲除后Hippo/YAP和c-MYC信号富集。连通图分析和药物再利用实验确定了pyroxamide可作为FRMD6缺失PC细胞的一种新的潜在疗法。最后,研究人员在ROSA26小鼠前列腺中建立了正交的Frmd6和Pten,或仅Pten(对照)敲除。12周后,Frmd6/Pten双基因敲除表现出高级别前列腺上皮内瘤变(HG-PIN)和过度增殖,而Pten单基因敲除仅出现常规PIN病变,并表现出较低程度的增殖。
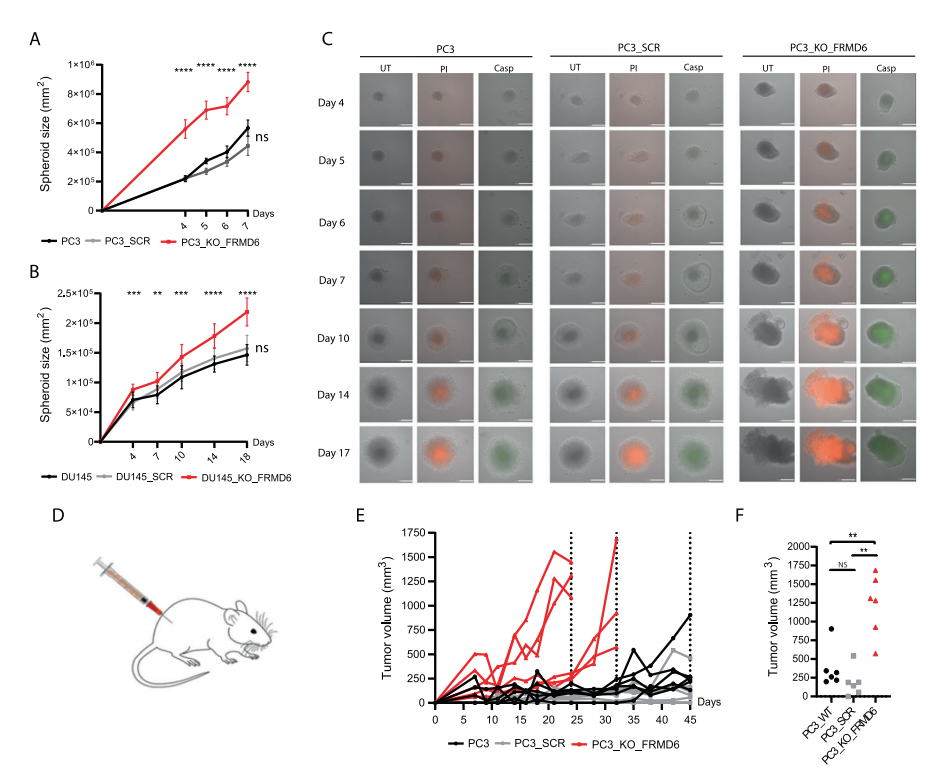
FRDM6抑制3D球状瘤和异种移植肿瘤的生长
最后,研究人员指出,他们的研究确定了FRMD6为PC中的新肿瘤抑制基因和预后生物标志物候选基因。
原始出处:
Jakob Haldrup, Siri H. Strand, Clara Cieza-Borrella et al. FRMD6 has tumor suppressor functions in prostate cancer. Oncogene. Nov 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制肿瘤#
136
#Gene#
78
#Oncogene#
113
前列腺癌相关研究,学习了,谢谢梅斯
137