花季少年左膝疼 痛苦难眠为哪般
2018-01-27 牛晓辉 郝林 骨肿瘤
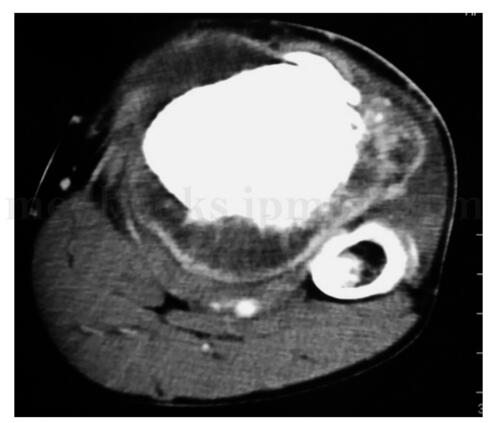
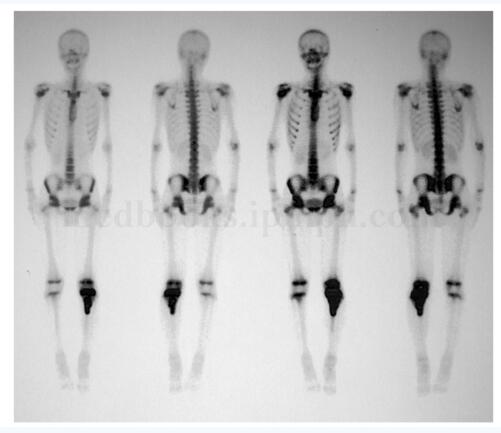
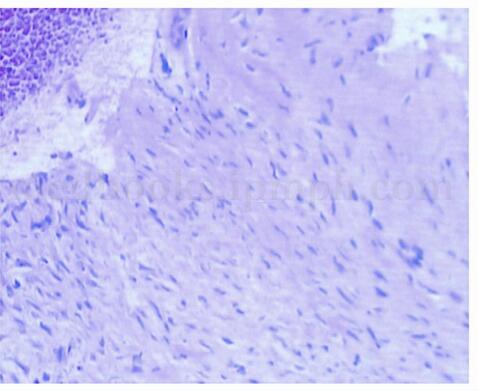
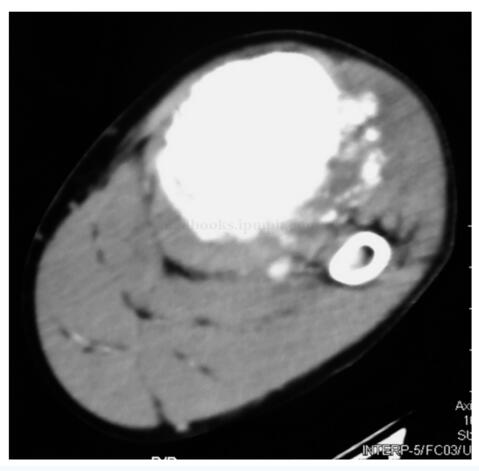
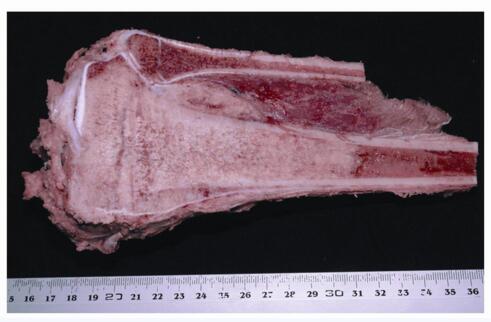
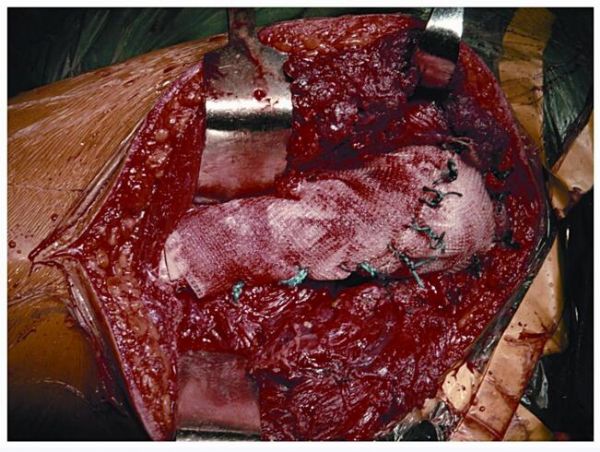
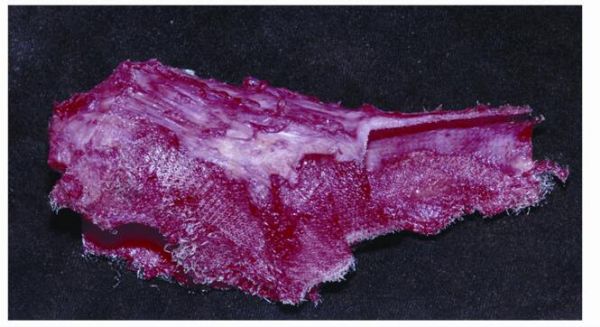
患者,男,17岁,主因左膝疼痛半年,门诊以胫骨近端肿瘤收入院。患者半年前扭伤左膝后感觉疼痛,未诊治,自行好转。5个月前再次出现左膝疼痛,夜间疼痛明显。3个月前疼痛加重,影响睡眠,并且左胫骨上端出现肿物并进行性增大。曾在大同市某医院行肿物抽吸涂片无阳性发现。遂来我院就诊,而收入院。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#花季少年#
65
学习了.蟹蟹
112
真的是学习了
76
学习
93
受益匪浅
107
谢谢分享.学习了
100
谢谢分享.学习受益匪浅
52