Ann Oncol:Tucatinib(图卡替尼)或安慰剂联合曲妥珠单抗+卡培他滨治疗经治晚期HER2+乳腺癌患者的疗效
2022-02-03 yd2015 MedSci原创
研究表明,延长随访时间,tucatinib(图卡替尼)联合用药仍持续改善HER2+转移性乳腺癌患者的预后。
HER2CLIMB研究是一项随机、双盲、安慰剂对照试验。纳入既往经治局部晚期或转移性HER2+乳腺癌患者,包括脑转移患者。随机2:1分配至 tucatinib(图卡替尼)或安慰剂联合曲妥珠单抗+卡培他滨治疗。初步分析结果表明,tucatinib(图卡替尼)联合曲妥珠单抗+卡培他滨治疗改善患者的预后。近期,Annals of Oncology杂志上更新了HER2CLIMB研究的最终OS结果。

HER2CLIMB研究纳入612名患者,其中 48%患者基线伴有脑转移。中位随访OS为29.6个月(比初步分析多了15.6个月)。Tucatinib(图卡替尼)联合治疗组的中位OS持续时间为24.7个月(95% CI: 21.6-28.9个月),而安慰剂联合治疗组的中位OS持续时间为19.2个月(95% CI: 16.4-21.4个月)(HR: 0.73, 95% CI: 0.59-0.90, P= 0.004)。Tucatinib联合组2年OS率为51% (95% CI: 46% - 56%),安慰剂联合组为40% (95% CI: 33% - 47%)。

OS差异
所有亚组的OS获益均偏向于Tucatinib联合组,并与整个研究人群的一致。
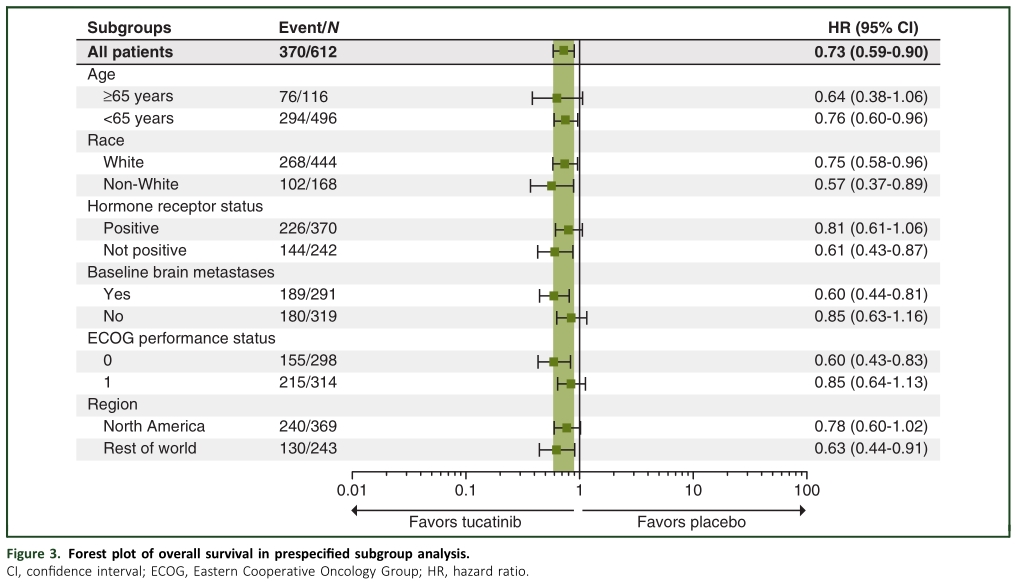
OS亚组分析
Tucatinib(图卡替尼)联合治疗组的中位无进展生存期(PFS)为7.6个月(95% CI: 6.9-8.3个月),而安慰剂联合治疗组为4.9个月(95% CI: 4.1-5.6个月)(HR: 0.57, 95% CI: 0.47-0.70, P<0.00001)。Tucatinib联合组1年PFS率为29% (95% CI: 24%-34%),安慰剂联合组为14% (95% CI: 9%-20%)。

PFS差异
Tucatinib(图卡替尼)联合用药耐受性良好,因不良事件停药率低。

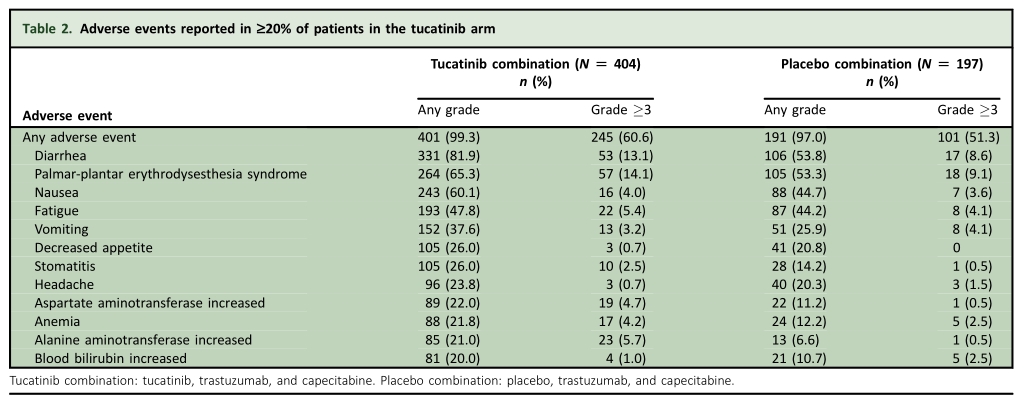
不良反应
综上,研究表明,延长随访时间,tucatinib(图卡替尼)联合用药仍持续改善HER2+转移性乳腺癌患者的预后。
原始出处:
Curigliano G, Mueller V, Borges V, Hamilton E, Hurvitz S, Loi S, Murthy R, Okines A, Paplomata E, Cameron D, Carey LA, Gelmon K, Hortobagyi GN, Krop I, Loibl S, Pegram M, Slamon D, Ramos J, Feng W, Winer E. Tucatinib versus placebo added to trastuzumab and capecitabine for patients with pretreated HER2+ metastatic breast cancer with and without brain metastases (HER2CLIMB): final overall survival analysis. Ann Oncol. 2021 Dec 23:S0923-7534(21)04879-1. doi: 10.1016/j.annonc.2021.12.005. Epub ahead of print. PMID: 34954044.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#晚期HER2+乳腺癌#
58
#Oncol#
78
#曲妥珠#
107
#卡培他滨#
89
#安慰剂#
96
#Tucatinib#
73
#乳腺癌患者#
72