BJU Int:组织学变异对pembrolizumab治疗的尿道癌患者结果的影响
2021-06-30 AlexYang MedSci原创
组织学变体在尿路上皮癌(UC)中已经有了很好的认识,并具有重要的诊断、预后和治疗意义。最常见的UC(VUC)组织学变体是鳞状细胞变体,大约20%的晚期UC存在此特征,其次是腺体特征,在16%至18%的
组织学变体在尿路上皮癌(UC)中已经有了很好的认识,并具有重要的诊断、预后和治疗意义。最常见的UC(VUC)组织学变体是鳞状细胞变体,大约20%的晚期UC存在此特征,其次是腺体特征,在16%至18%的晚期UC中存在。具有鳞状分化的UC是一种更具侵略性的类型,通常是由于伴随有较高等级的UC;与PUC相比,诊断时阶段较晚。另外,较少见的变体,如肉瘤型和浆细胞型变体,其预后最差。

近期,有研究人员评估了组织学变异对耐化疗的尿路上皮癌(UC)患者生存期和对pembrolizumab治疗反应的影响。

研究人员回顾了755名接受pembrolizumab治疗的晚期UC患者的医疗记录。患者分为纯UC(PUC)和各变异体,并使用倾向得分匹配(PSM)比较了各组之间的最佳总反应(BOR)和总生存期(OS)。
结果发现,总的来说,147名(19.5%)患者存在组织学变异UC(VUC)。在PSM之后,VUC和PUC患者的客观反应率(ORR,24.5% vs 17.3%,p=0.098)和疾病控制率(DCR,36.7% vs 30.2%,p=0.195)均没有显著差异。此外,VUC与PUC相比,其死亡风险相似(HR,0.90;95%CI,0.68至1.20;p=0.482)。鳞状VUC是队列中最常见的变异体,与PUC或非鳞状VUC相比,其ORR、DCR和OS相当。与PUC患者相比,肉瘤状VUC患者(n=19)的ORR(36.8%,p=0.031)、DCR(52.6%,p=0.032)和OS(HR 0.37;95%CI 0.15至 0.90;p=0.023)明显更好。
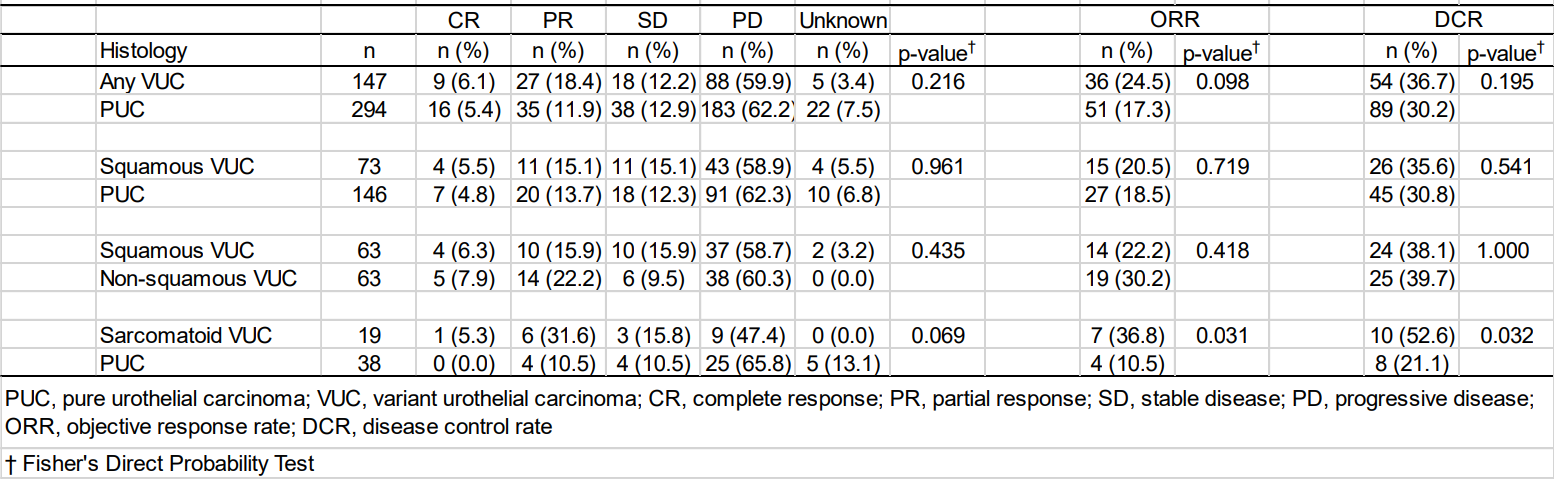
倾向性得分匹配后客观反映率和疾病控制率情况
综上所述,变异组织学的存在似乎并不影响化疗耐药UC患者使用pembrolizumab后的BOR或OS。与PUC相比,肉瘤型UC患者取得了良好的反应和生存率。
原始出处:
M Kobayashi, S Narita, Y Matsui et al. Impact of histological variants on outcomes in patients with urothelial cancer treated with pembrolizumab: a propensity score matching analysis. BJU Int. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#mAb#
44
#组织学#
46
#Pembro#
64
#尿道#
51
#Pembrolizumab#
43
#变异#
35
#尿道癌#
42
#PE#
31