Neurology:血清S100B浓度作为机械取栓后替代结局参数
2021-10-13 MedSci原创 MedSci原创
机械取栓后S100B血清浓度可反应缺血组织损伤的程度。它可以被快速评估,独立于脑成像结果和临床结局量表。在进一步研究中进行前瞻性验证后,它可以在临床常规和介入试验中提供客观的替代结局参数。
近日,神经病学领域权威取杂志Neurology上发表了一篇研究文章,该研究旨在明确血清S100B蛋白浓度作为急性缺血性卒中患者机械取栓后星形胶质细胞组织损伤的客观生物标志物替代物。

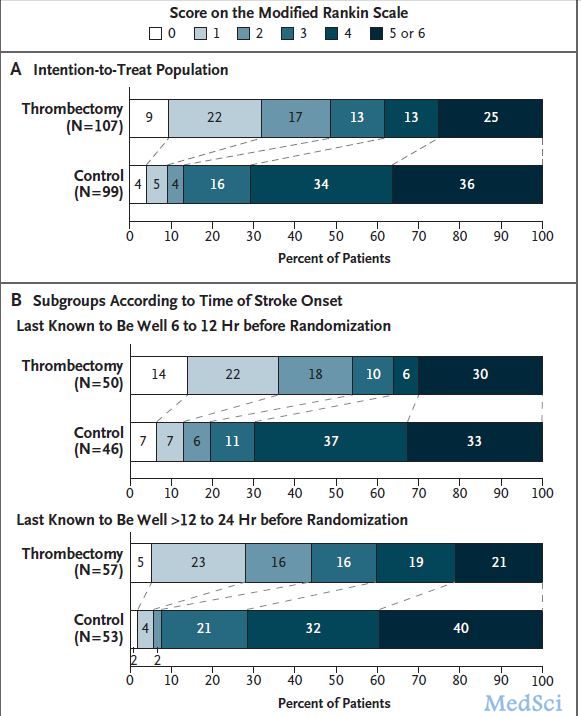
这项前瞻性的两中心研究招募了因大血管闭塞而接受机械取栓治疗的急性大脑中动脉梗死患者。研究人员在受试者干预后第2天收集血样并使用ELISA技术分析S100B血清浓度。随访通过脑成像检查确定梗死面积,并在90天时根据改良的Rankin量表(mRS)评估功能结局。
该研究共纳入了171名患者(平均年龄±SD:70±14岁,42%为女性)。S100B水平与梗死面积相关。与预后不良的患者(mRS评分2-6)相比,干预后第2天的S100B浓度中位数在90天时预后良好的患者(mRS评分为0-1)较低(中位数为0.10µg/L[IQR为0.07-0.14] vs. 0.20µg/L[0.11-0.48],p<0.001)。
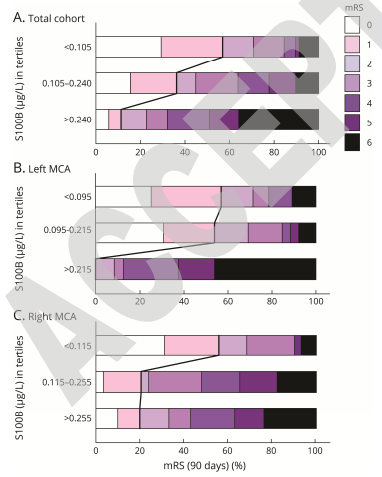
年龄较小(OR为1.120[95%CI为1.068-1.174;p<0.001),症状出现后24小时NIHSS降低(OR为1.232[95%CI为1.106-1.372;p<0.001),S100B血清浓度降低(OR为1.11.165[95%CI为1.1.165]]p=0.004)与有利的结局独立相关。
由此可见,机械取栓后S100B血清浓度可反应缺血组织损伤的程度。它可以被快速评估,独立于脑成像结果和临床结局量表。在进一步研究中进行前瞻性验证后,它可以在临床常规和介入试验中提供客观的替代结局参数。
原始出处:
Sebastian Luger.et al.Role of S100B Serum Concentration as a Surrogate Outcome Parameter After Mechanical Thrombectomy.Neurology.2021.https://doi.org/10.1212/WNL.0000000000012918
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#S100B#
62
#Neurol#
62
#取栓#
68
#浓度#
61
#机械取栓#
68
学习了!
78
已读已读已读已读已读已读已读已读已读已读已读已读已读
78