样本量计算:成组设计的病例对照研究
2017-09-01 佚名 医咖会微信号
样本量的计算直接影响着临床试验的阴性或者阳性,而如何计算样本量实现效益与经济的平衡,是非常关键的问题。本公众号将持续转载报道医咖会整理的样本量计算系列推文,以便掌握样本量计算方法,助力临床试验设计
样本量的计算直接影响着临床试验的阴性或者阳性,而如何计算样本量实现效益与经济的平衡,是非常关键的问题。本公众号将持续转载报道医咖会整理的样本量计算系列推文,以便掌握样本量计算方法,助力临床试验设计
1、问题与数据
某研究者拟进行一项病例对照研究,探讨吸烟与肺癌的关系。选择肺癌患者为病例组,选择非肺癌患者为对照组。预期比值比OR=2.0,对照组人群中的吸烟率约为20%,设α=0.05,β=0.10。拟定病例组和对照组采用相等样本量,请问如何估计病例组和对照组的样本量?
2、对问题的分析
研究者的设计为病例对照研究,并且病例组和对照组各为一组,因此该设计类型为成组设计的病例对照研究。病例对照研究中,我们把想要探讨的危险因素称为暴露。
如果我们关注的暴露因素有多个,则计算样本量的原则一般如下:1)以最想关注的那个暴露因素计算得到的样本量为准;2)计算所有的暴露因素应有的样本量,然后取最大值。
3、PASS软件计算样本量方法
1)选择Proportions→Two Independent Proportions→Test (Inequality)→Test for Two Proportions[Odds Ratios]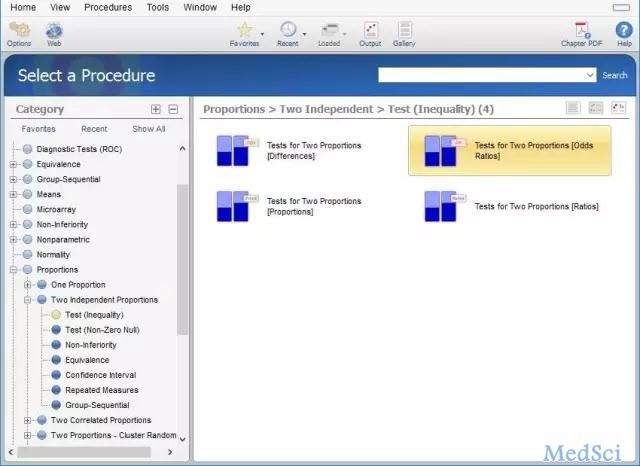
2)Find (Solve for)中选择N1,Power (1-Beta)中选择0.9,Alpha (Significance Level)中选择0.05,N2 (Sample Size Group 2)中选择Use R,R (Sample Allocation Ratio)中选择1.0,OR1 (Odds Ratio|H1=O1/O2)中填入2.0,P2 (Control Group Proportion)中选择0.2。其它选择为默认选项后,点击RUN。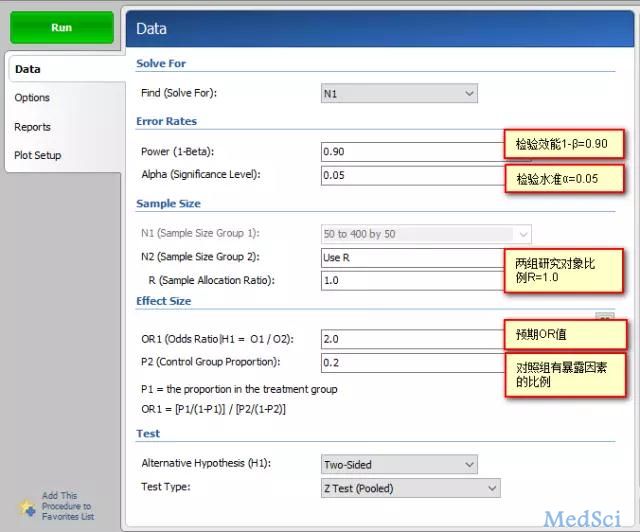
4、结果解读
PASS软件给出了样本量计算的结果、参考文献、报告中的名词定义和总结性描述。在样本量计算结果中我们需要关注以下两列:
1)Sample Size Grp 1 (N1):病例组样本量。本研究的病例组需要230例研究对象。
2)Sample Size Grp 2 (N2):对照组样本量。本研究的对照组需要230例研究对象。
5、撰写结论
本研究为成组设计的病例对照研究。病例组为肺癌患者,对照组为非肺癌患者,吸烟为主要观察的暴露因素。根据既往文献报道,对照组(非肺癌患者)人群中的吸烟率约为20%。预期OR=2.0,设α=0.05,β=0.10。利用PASS 11软件计算得到病例组和对照组的样本量N1=N2=230例。假定研究对象的无应答率为10%,则需样本量N1=N2=230÷0.9=256例。假定问卷合格率为90%,则共需样本量为N1=N2=256÷0.9=284例。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#病例对照研究#
76
#病例对照#
90
#样本#
76
#对照#
96
#样本量#
115