BMJ:广医附一院何建行教授团队发文:EGFR突变晚期非小细胞肺癌更佳一线治疗方案
2019-10-09 肿瘤资讯 肿瘤资讯
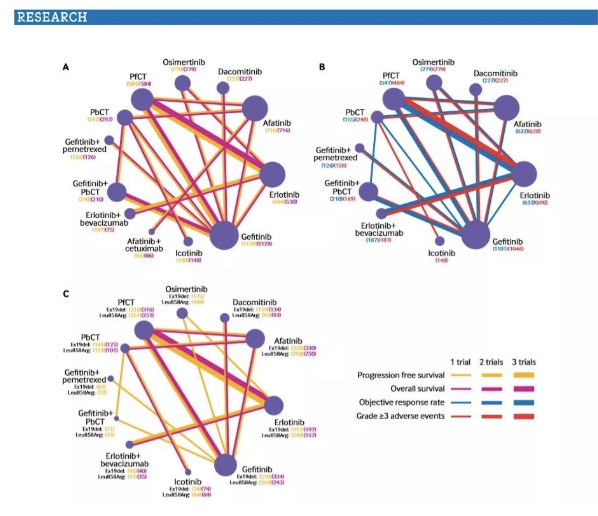
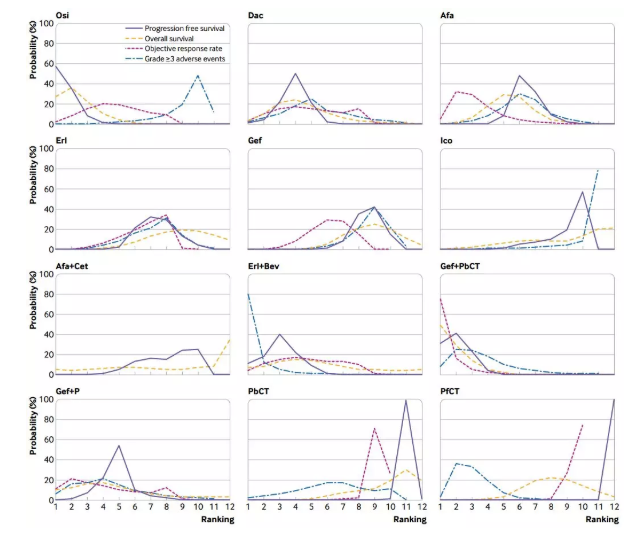
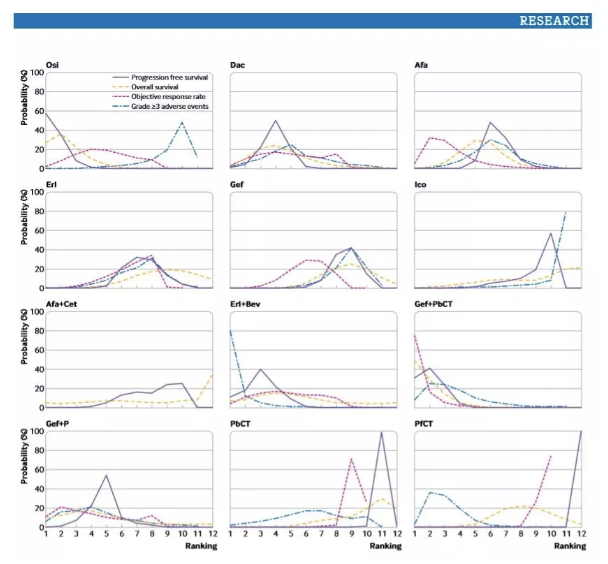
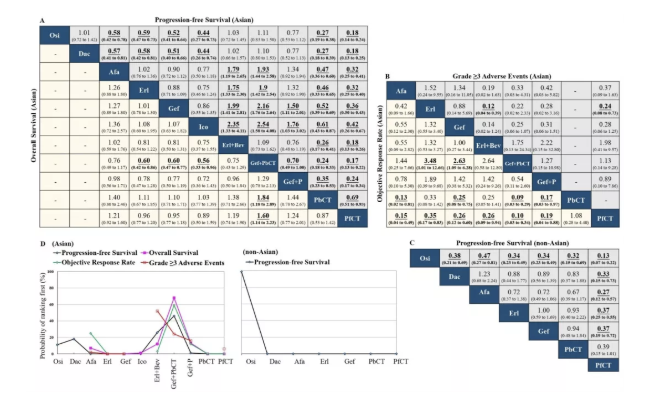
肺癌是全球发病率和死亡率最高的恶性肿瘤,约50%的亚洲患者和11%~16%的西方患者存在表皮生长因子受体(EGFR)敏感突变(主要包括Exon 19 Del和21 L858R);对这类患者,NCCN国际指南目前推荐一线使用表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKI)的靶向治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
77
#何建行#
109
#治疗方案#
84
#BMJ#
86
#GFR#
108
原来是meta analysis
120