J Am Acad Dermatol:利妥昔单抗治疗的天疱疮患者,复发的生物标志物有哪些?
2017-09-27 MedSci MedSci原创
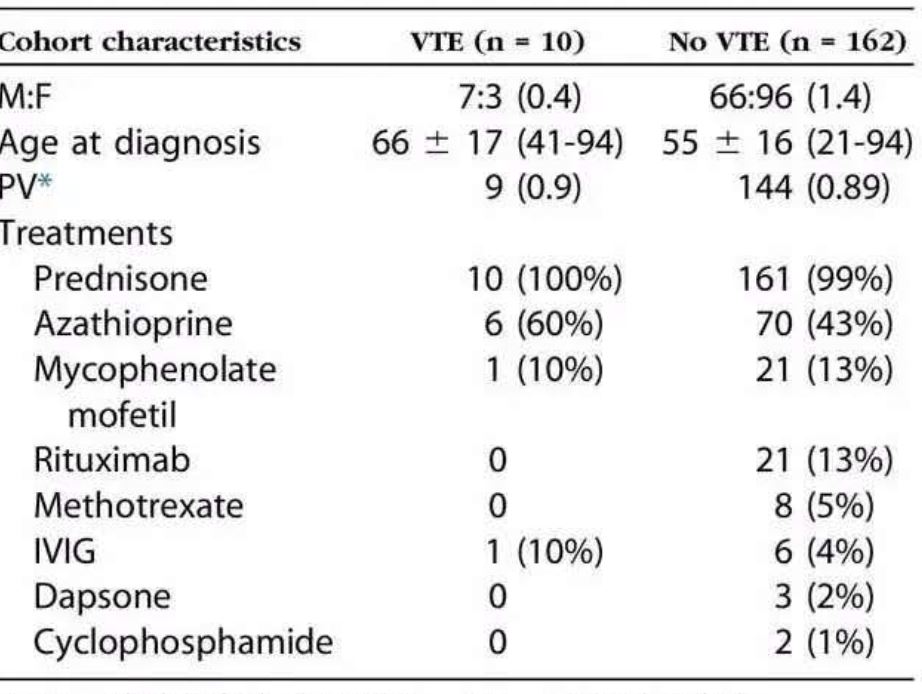
背景:利妥昔单抗是治疗天疱疮的有效方法,但患者在接受治疗后常出现复发。目的:本研究旨在识别能利妥昔单抗治疗天疱疮后天能预测复发的生物标志物。方法:这是一项回顾性队列研究,研究人员回顾并分析了62例接受利妥昔单抗治疗的天疱疮患者的临床评分水平和生物标志物数据,包括CD19+B细胞、CD4 + T细胞和桥粒芯糖蛋白1(Dsg1)抗体、桥粒芯糖蛋白3(Dsg3)抗体水平。研究人员采用了时间变异的拓展Ka
背景:利妥昔单抗是治疗天疱疮的有效方法,但患者在接受治疗后常出现复发。目的:本研究旨在识别能利妥昔单抗治疗天疱疮后天能预测复发的生物标志物。方法:这是一项回顾性队列研究,研究人员回顾并分析了62例接受利妥昔单抗治疗的天疱疮患者的临床评分水平和生物标志物数据,包括CD19+B细胞、CD4 + T细胞和桥粒芯糖蛋白1(Dsg1)抗体、桥粒芯糖蛋白3(Dsg3)抗体水平。研究人员采用了时间变异的拓展Kaplan Meier生存分析和扩展的Cox模型进行数据分析。结果:在B细胞增殖之前的复发是罕见的。单因素分析显示低水平的CD4计数(<400细胞/μl)能预测复发(p<0.001)。在患有皮肤疾病的患者中,DSG1测试的阳性结果(> 20 IU)预测复发(风险比,6.40;P = 0.019);在患有皮肤和粘膜疾病的患者中,Dsg3测试的阳性结果(> 20 IU)预测复发(风险比,32.92;P<0.001。)。多变量分析显示,CD4值每增加200,复发的风险比降低35%(P=0.029)。在患有皮肤疾病的患者中,DSG1测试的阳性结果增加了12.32个系数的复发风险(P = 0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ACA#
77
#利妥昔#
57
#标志物#
70
#生物标志#
0
#生物标志#
68