Clin Gastroenterol H:胃食管反流病的又一诊断标志-食管上皮厚度
2016-10-24 xing.T MedSci原创
由此可见,该研究基于336例经常出现上消化道症状患者的数据分析,总上皮厚度是诊断GERD的一个很重要组织学标志。
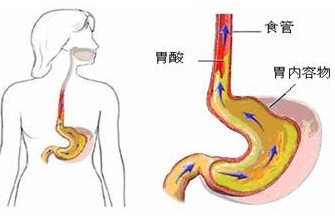
目前,组织学标准被细化用于诊断胃食管反流病(GERD)。消化病领域权威杂志《Clinical
Gastroenterology and Hepatology》发表了一篇研究文章,旨在评估食管上皮厚度在GERD诊断的作用。
在欧洲和加拿大的成年人群中,研究者征集以经常出现上消化道症状并且未服用质子泵抑制剂的患者为研究对象进行Diamond研究(NCT 00291746),并对Diamond研究的数据进行了深入挖掘。GERD的诊断基于以下1个或更多的临床表现:反流性食管炎、胃酸暴露的病理性食管和/或胃酸相关的阳性症状。非糜烂性反流病诊断依据为胃酸暴露的病理性食管和/或胃酸相关的阳性症状,但无反流性食管炎。研究者收集和评估了336例患者Z线0.5厘米和2厘米以上的活检结果,通过德国和意大利的活检病理中心(分别为258例和195例)进行独立分析。主要指标是GERD的组织学诊断标准的准确性,通过内镜和pH监测来确定。
研究者发现:基底细胞层增厚的位置以及总上皮厚度是诊断GERD的最佳的诊断标准;它还明确了Z线0.5厘米和2厘米以上的非糜烂性反流病、反流性食管炎以及胃酸暴露的病理性食管情况。基底细胞层厚度和存在扩张的细胞内间隙并不能诊断为GERD。在测试的诊断标准中,两个活检病理中心给出的最好的诊断指标是评估Z线0.5厘米和2厘米以上总上皮厚度。
由此可见,基于336例经常出现上消化道症状患者的数据分析,总上皮厚度是诊断GERD的一个很重要组织学标志。
原始出处:
Michael Viethcor,et al. Epithelial Thickness is a Marker of Gastroesophageal Reflux Disease. clinical gastroenterology and hepatology 2016.2016 Nov;14(11):1544-1551.e1.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胃食管#
71
#GAS#
51
#反流病#
65
#AST#
72
#Gastroenterol#
76
#诊断标志#
74
学习了,长知识了
94
研究好
101
#胃食管反流#
98
#食管#
87