Oncotarget:新型无毒副作用疗法可治疗多种癌症
2016-05-20 生物谷 梅斯医学
近日,刊登于国际杂志Oncotarget上的一项研究论文中,来自迈阿密大学米勒医学院的研究人员通过研究开发了一种新型无毒疗法来治疗多种类型的癌症;这种新型疗法基于2-脱氧葡萄糖(2-Deoxy-D-glucose,2-DG)和胆固醇药物非诺贝特的组合性疗法而开发。
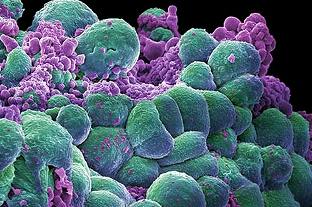
图片摘自:www.researchandinnovation.ie
近日,刊登于国际杂志Oncotarget上的一项研究论文中,来自迈阿密大学米勒医学院的研究人员通过研究开发了一种新型无毒疗法来治疗多种类型的癌症;这种新型疗法基于2-脱氧葡萄糖(2-Deoxy-D-glucose,2-DG)和胆固醇药物非诺贝特的组合性疗法而开发。
研究者Theodore Lampidis说道,在所有实体瘤的内部核心中发现的癌细胞中的氧气水平都异常低,而正因为如此,这些癌细胞都依赖于糖酵解过程,糖酵解是一种通过分解葡萄糖来产生能量的代谢过程,这些癌细胞天生生长缓慢,而且其对常规的癌症疗法均产生耐药性,比如放疗和化疗等。
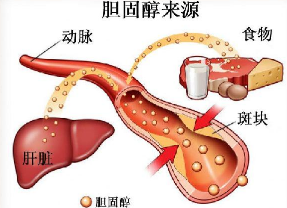
本文研究中,研究人员发现,阻断醣酵解过程的“假糖”,比如2-脱氧葡萄糖就会有选择性地饿死生长缓慢的癌细胞,同时会保留正常细胞,而正常细胞是利用其它能源来产生能量,比如脂肪和蛋白质,因为这些物质处于完全氧化状态。尽管目前该项研究还处于I期临床试验阶段,但2-脱氧葡萄糖结合常规抗癌药物的联合疗法被证明可以成功抵御癌细胞,而化疗产生的毒性副作用仍然是一个问题;本文研究中,研究人员就将药物非诺贝特同2-脱氧葡萄糖进行结合,药物非诺贝特是一种已经安全应用超过40年的用于降低人类机体胆固醇和甘油三酯水平的药物;研究结果表明,非诺贝特同2-脱氧葡萄糖的结合可以在不产生毒性副作用的前提下有效靶向作用肿瘤细胞。
研究者发现,当非诺贝特和2-脱氧葡萄糖的特殊结合就可以同时诱发两种压力效应,即能量压力和内质网应激压力,这两种压力均不能被大部分癌症所克服。由于癌细胞的自由生长及异常的微环境所致,其往往要比正常健康细胞面临更多压力,此外,2-脱氧葡萄糖还会利用万能的癌细胞特性即便增加葡萄糖摄入,当同非诺贝特结合后,组合性疗法就可以有效利用癌细胞的第二个特点即增加压力,来对癌细胞进行精确狙杀。
最后研究者Lampidis说道,我们认为这种新型的组合性疗法或可帮助治疗多种类型的癌症,对于后期开发更多有效的个体化癌症疗法提供了一定的研究基础和思路。

原始出处:
Huaping Liu1,et al.Combining 2-Deoxy-D-glucose with fenofibrate leads to tumor cell death mediated by simultaneous induction of energy and ER stress.Oncotarget.DOI: 10.18632/oncotarget.9263
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#副作用#
63
#毒副作用#
83
#target#
75
拜读,好文
108
思路是好的,希望能够获得成功。
162