JACC:PCI术后输注比伐卢定可改善预后
2019-02-22 不详 MedSci原创
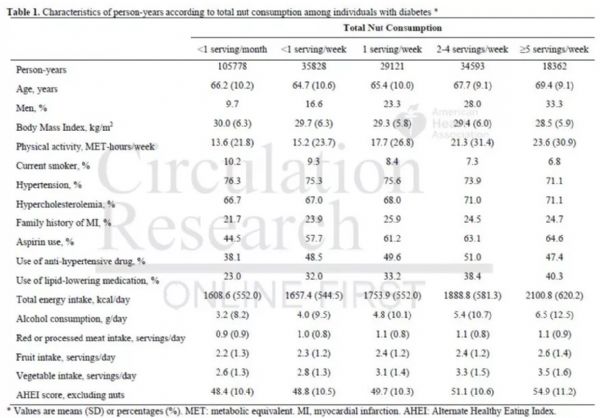
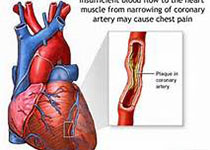
急性冠脉综合征(ACS)患者经皮冠脉介入(PCI)术后比伐卢定长期输注的价值和意义尚不清楚。本研究的目的旨在评估ACS患者PCI术后全或低比伐卢定输注的安全性和有效性。本研究纳入了MATRIX 临床研究中的患者,主要终点事件是紧急靶血管血运重建、明确的支架血栓形成或不良临床事件的复合事件。最终,共纳入分析了3610名患者,其中1799名患者接受有PCI术后比伐卢定输注,1811名没有。有612名患
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PCI术#
93
#比伐卢定#
85
#JACC#
61
我认为不见得可以改善
123
学习了,长知识
112
#ACC#
0
#PCI术后#
69
为作品点赞!认真学习了,把经验应用于实践,为患者解除病痛。
112