Eur J Heart Fail:循环蛋白作为老年人心力衰竭的预测因子!
2018-02-11 xing.T MedSci原创
由此可见,蛋白质组学分析发现凋亡相关蛋白、炎症、基质重塑和纤维蛋白溶解与老年人心力衰竭之间新的相关性。该研究的结果支持进行额外的研究以调查的潜在的机制和该研究结果的临床应用。
近日,心血管领域权威杂志European Journal of Heart Failure上发表了一篇研究文章,该研究旨在利用包含80种与心血管疾病相关的蛋白的蛋白质表达谱来确定心衰新的危险标志物。
研究人员对两个基线无心衰的社区老年人群前瞻性队列进行蛋白组学谱(接近延伸法):在乌普萨拉老年人血管系统的前瞻性调查[PIVUS,n=901,年龄中位数为70.2(四分位距为70-70.3)岁,80次事件]和乌普萨拉成年男人纵向研究[ULSAM,n=685,年龄中位数为77.8(四分位距为76.9-78.1)岁,90次事件]。
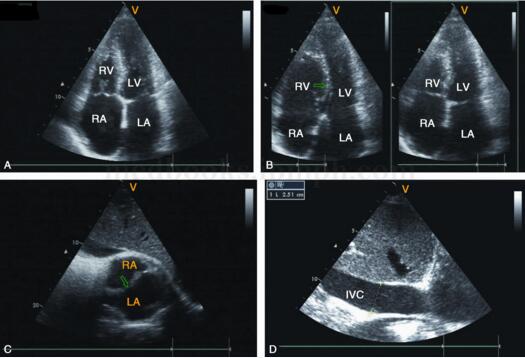
在PIVUS发现队列中,调整年龄和性别后,研究人员发现了二十九个与心衰事件有关的蛋白质。在ULSAM队列中有十八个蛋白可以重复出来。在两组汇总分析中,在对已知的危险因素进行调整后,九种较高水平的蛋白质与心衰相关:生长分化因子15(GDF-15)、T细胞免疫球蛋白及粘蛋白域1(TIM-1)、肿瘤坏死因子相关的凋亡诱导配体受体2(TRAIL-R2)、spondin-1(SPON1)、基质金属蛋白酶-12(MMP-12)、卵泡抑素(FS)、尿激酶型纤溶酶原激活物受体(u-PAR)、骨保护素(OPG)和致瘤抑制素2(ST2)。其中,GDF-15、u-PAR、MMP-12、TRAIL-R2、SPON1和FS与基线时左室收缩功能恶化超声心动图指标相关,而只有TIM-1与恶化的舒张功能呈正相关(所有P<0.02)。
由此可见,蛋白质组学分析发现凋亡相关蛋白、炎症、基质重塑和纤维蛋白溶解与老年人心力衰竭之间新的相关性。该研究的结果支持进行额外的研究以调查的潜在的机制和该研究结果的临床应用。
原始出处:
Markus Stenemo,et al. Circulating proteins as predictors of incident heart failure in the elderly.Eur J Heart Fail.2018. http://onlinelibrary.wiley.com/doi/10.1002/ejhf.980/full
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#循环蛋白#
92
#预测因子#
83
#ART#
77
#HEART#
87
学习了.谢谢分享
104
谢谢分享学习
98