Nature:华人学者Nature重磅!儿童癌症大不同 与成人突变重合率不到一半
2018-03-01 佚名 学术经纬
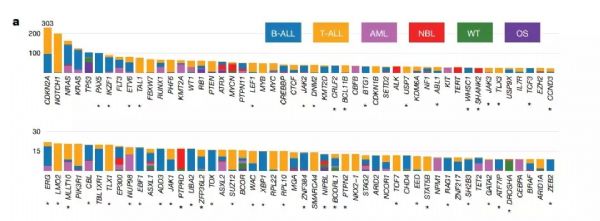
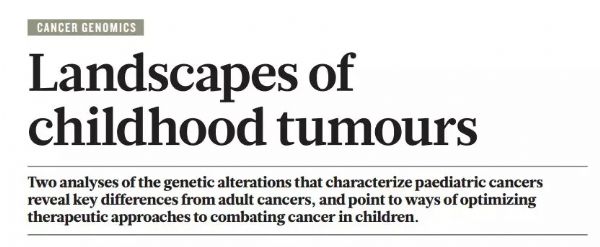
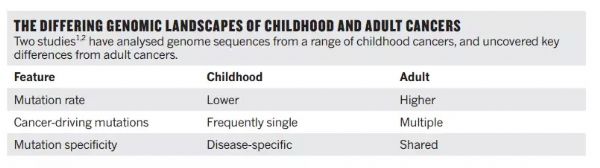
今日,知名学术刊物《自然》背靠背在线刊发了两篇重磅论文,报道了在儿童中进行的首次泛癌症基因组分析。这些分析对于了解儿童与成人的癌症区别有着很重要的意义,并有望为儿童带来更为精准的疗法。我们很高兴看到St.Jude儿童研究医院的JinghuiZhang教授主导了其中的一项研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
39
#儿童癌症#
51
#重磅#
31
#华人#
43
#华人学者#
47