JACC:家族性高胆固醇血症患者通过药物很难达到LDL-C的正常水平
2016-03-15 崔倩 译 MedSci原创
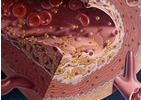
家族性高胆固醇血症(FH)是最常见的遗传性疾病,与早发动脉粥样硬化性心血管疾病(ASCVD)有关。关于达到治疗靶点的数据很少;大量反映现实生活的临床实践的注册可以唯一提供此信息。在一个大的国家登记注册中,研究人员试图评估低密度脂蛋白胆固醇(LDL-C)的治疗目标在FH患者的情况。该SAFEHEART研究(西班牙家族性高胆固醇队列研究)是一项大型的,分子定义的杂合子FH患者的持续的注册研究,在西班牙
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
50
好,学习了
119
很多疾病都具有遗传性!
154
#ACC#
73
#高胆固醇血症#
57
#LDL#
45
#家族性#
58
以前有相似报到
169
降低LDL至正常太难
131