Cardiovasc Diabetol:冠状动脉疾病患者的血清Nesfatin-1和DPP4水平及其相关性
2021-08-15 Nebula MedSci原创
血清DPP4水平在CAD患者中升高,而血清Nesfatin-1水平与CAD的发生率和严重程度均具有负性相关性
Nesfatin-1(一种新型脂肪因子)和二肽基肽酶 4(DPP4,一种哺乳动物丝氨酸蛋白酶),都是动脉粥样硬化的有效因素。在该横断面研究中,研究人员调查了血浆Nesfatin-1和DPP4是否与冠状动脉疾病(CAD)的患病率和严重程度相关,无论是否患有糖尿病(DM)。
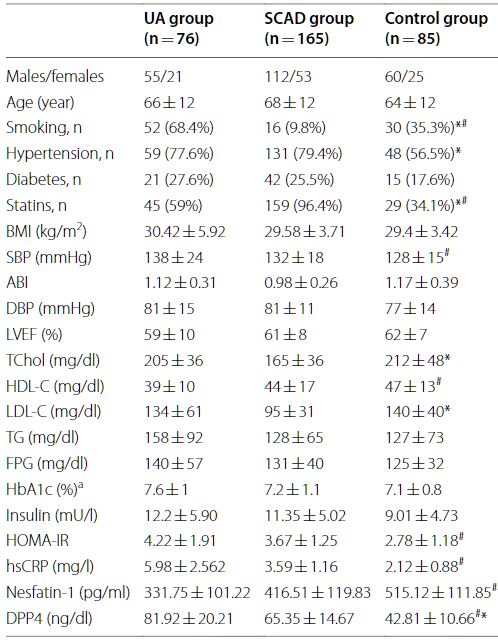
研究人员连续招募了240位有显著CAD的患者(既往进行过血运重建或血管造影证实冠状动脉狭窄>50%),其中76位表现为不稳定心绞痛(UA),165位表现为稳定型慢性CAD(SCAD)。此外,还招募了85位至少有两个心血管危险因素但无明显CAD的患者作为对照。采用冠脉造影评估CAD的严重程度。另外,还分析了受试者的临床参数、血糖和血脂、高敏CRP (hsCRP)、Nesfatin-1和DPP4 水平。
各研究组的基本特征
各组间受试者的年龄、性别、高血压和糖尿病分布均无明显差异。与对照组相比,两个CAD组(UA组和SCAD组)的Nesfatin-1水平均较低。UA组和SCAD组之间的Nesfatin-1水平无明显差异。UA组和SCAD组的DPP-4水平均显著高于对照组。这些组间差异在非糖尿病受试者中保持不变。
Nesfatin-1与hsCRP与冠状动脉疾病的存在相关
Nesfatin-1与hsCRP(r=-0.287,p=0.036)、HOMA-IR(r=-0.587,p=0.007)和高脂血症(r=-0.331,p=0.036)相关。在单变量分析中,DPP4与hsCRP(r=0.353,p<0.001)和FPG(r=0.202,p=0.020)显著相关,但在多变量回归分析中,这些相关性消失。Nesfatin-1与CAD的严重程度呈负相关(r=-0.511,p<0.001),但DPP4与CAD的严重程度无相关性。
总而言之,血清DPP4水平在CAD患者中升高,而血清Nesfatin-1水平与CAD的发生率和严重程度均具有负性相关性。这些结果与合并糖尿病与否无关。此外,Nesfatin-1和DPP4均与hsCRP具有很强的相关性。
原始出处:
Kadoglou, N.P.E., Korakas, E., Lampropoulos, S. et al. Plasma nesfatin-1 and DPP-4 levels in patients with coronary artery disease: Kozani study. Cardiovasc Diabetol 20, 166 (2021). https://doi.org/10.1186/s12933-021-01355-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
45
#BET#
47
#相关性#
42
#fat#
60
#ASC#
52
#疾病患者#
54
#冠状动脉疾病#
58
#DPP4#
52
学习了
92
棒
74