高尿酸血症肾脏损害的研究进展
2015-01-28 施映枫 王莉 徐柳青 庄守纲 严海东 刘娜 中华肾脏病杂志
尿酸是人类嘌呤化合物代谢的终末产物,嘌呤代谢紊乱可增加高尿酸血症的发生率,在正常嘌呤饮食状态下,非同日两次空腹血尿酸水平男性高于420μmol/L,女性局于360μmol/L,即称为高尿酸血症(hyperuricemia)。 最近的13项流行病学研究也评价了血尿酸水平与慢性进展性肾病之间的关系,其中8项研究证实了血尿酸与肾病进展相关。

尿酸是人类嘌呤化合物代谢的终末产物,嘌呤代谢紊乱可增加高尿酸血症的发生率,在正常嘌呤饮食状态下,非同日两次空腹血尿酸水平男性高于420μmol/L,女性局于360μmol/L,即称为高尿酸血症(hyperuricemia)。
最近的13项流行病学研究也评价了血尿酸水平与慢性进展性肾病之间的关系,其中8项研究证实了血尿酸与肾病进展相关。
在规模最大的1项研究中,随访对象为美国肾病数据库系统的177570例患者,随访时间长达25年,研究发现,血尿酸水平增高的患者发生慢性肾脏病(CKD)的风险是尿酸正常患者的2.14倍。
同样,在人群动脉粥样硬化危险性试验中,血尿酸每增高59.5μmol/L,CKD发生的风险增加7%~11%。Liu等的1项研究选取了788例接 受了冠脉造影但肾功能正常的受试患者,将其分成高尿酸血症组和血尿酸正常范围组,研究表明高尿酸血症是患者发生急性肾损伤的高危因素,并且大部分患者需要 肾脏替代治疗。
在国内,高尿酸血症患者中,并发肾病的发生率达15.1%,而血尿酸正常的人群高尿酸血症肾损害的发生率仅为2.9%。上述流行病学研究在很大程度上都说明高尿酸血症是肾脏疾病发生的一个重要危险因素。
我们课题组致力于CKD发生机制研究,在表观遗传、细胞信号通路调控CKD进展方面做了部分工作,近期我们更加关注高尿酸血症肾脏损害发生机制及防治研究。因此,本文将针对高尿酸血症形成的病因及高尿酸血症肾损害的发生机制研究的最新进展作一综述。
一、局尿酸血症的病因
高尿酸血症按照血尿酸升高的原因不同,可分为原发性高尿酸血症和继发性高尿酸血症。原发性高尿酸血症发生机制近期的研究热点集中在尿调节素(UM0D)基因突变,不同国家与地区均有新的研究报道。
(一)原发性高尿酸血症
在原发性高尿酸血症发生机制的研究中,国内外学者均致力于UM0D基因突变研究。UM0D作为一种糖蛋白,其相对分子质量为95000,健康人群每天 分泌的正常值为20 70mg,是尿液中占比重最多的蛋白。UM0D基因的16号染色体12.3区域(16P12.3)突变可以导致“尿调节素贮积病”。
研究证明,家族性幼年高尿酸血症性肾病I型(family with juvenile hyperuricemic nephropathy1,FJHN1)是常染色体显性遗传疾病,其是一种与UMOD基因突变密切有关的疾病,由异常的UM0D在管状细胞中沉积所导致, 临床主要表现为高尿酸血症肾损害和痛风性关节炎最近,韩国和日本学者应用基因检测方法,又发现了UM0D基因的新的突变位点(c.187T>C)和 (T688C)。
1.尿酸生成过多:
即内源性尿酸生产过多,规定在超过5d低嘌呤饮食(<3mg/d)的情况下,患者尿液中尿酸含量仍大于600mg者就定义为尿酸生产过多。
其机制可能与酶基因突变有关,在尿酸生成过程中起促进作用的一些酶数量与活性增加和(或)起抑制作用的相关酶的数量和活性降低。
相关酶基因有以下几类:次黄嘌呤、鸟嘌呤核糖转换酶(HGPRT);磷酸核糖焦磷酸酰胺移换酶(PRPP)合成酶;次黄嘌呤、黄嘌呤氧化酶(XO);N5,N10-亚甲基四氢叶酸还原酶(MTHFR);葡萄糖-6-磷酸酶等
2.尿酸排泄减少:
尿酸盐作为极性分子,它不能像水或者其他离子型电解质一样自由的通过细胞膜,因此,尿酸盐在近曲肾小管处的重吸收和分泌过程需要转运蛋白的协助,完成离子通道的主动转运过程。
而已知的相关转运蛋白有:(1)位于近段肾小管的尿酸特异性转运蛋白(UAT);(2)有机阴离子转运蛋白家族,其中0AT1位于近端肾小管S2段的基底侧,0AT3位于近段肾小管、髓襻升支粗段;(3)位于肾小管刷状缘侧的人尿酸转运蛋白URAT1。
这些处于不同部位的转运蛋白分别担负着尿酸盐的重吸收、分泌等功能。任何参与尿酸转运的蛋白质基因突变和(或)基因多态性改变、功能障碍都会导致其表达量变化或功能失调,最终导致尿酸排泄减少。
URAT1是调控尿酸转运的最重要的蛋白之一,编码URAT1的基因是SLC22A12。Ichida等对日本人群的基因研究发现SLC22A12基因的变异可导致血尿酸水平下降。
Hosoyamada等利用pMClneo-polyA改变小鼠的SLC22A12基因外显子的14位点,成功制备出SLC22A12基因敲除小鼠, 结果发现基因敲除小鼠尿液中尿酸盐和肌酐的浓度显著高于正常对照组,血液中的尿酸盐的浓度与正常组比较无差异,研究表明基因敲除小鼠的肾脏尿酸重吸收功能 减弱。
(二)继发性高尿酸血症
1.尿酸生成过多:
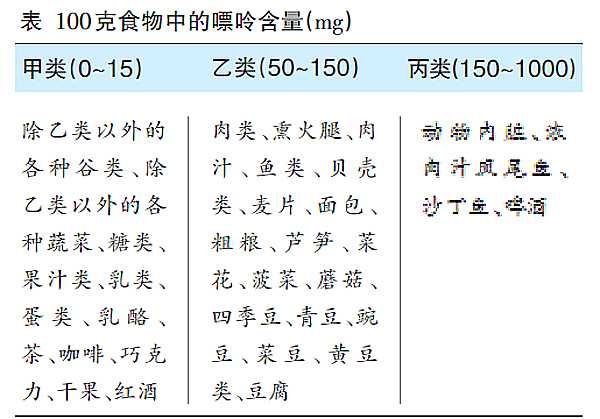
即获得性尿酸增加。(1)嘌呤代谢增加:血液疾病如慢性溶血性贫血、红细胞增多症、骨髓增生性疾病以及在一系列化疗或放疗过程时。同时过度的运动和处 在癫痫状态的患者,其肌肉ATP的降解速度加快,导致嘌呤代谢增高。(2)核苷酸转化增加:常见于白血病、多发性骨髓瘤、淋巴瘤等血液疾病的化疗、放疗治 疗中,大量破坏的白细胞加快了核酸的代谢,引发继发性高尿酸血症。(3)高嘌呤饮食。(4)酗酒。(5)过度肥胖。
2.尿酸排泄减少:
即肾脏排泄尿酸的量减少。尿酸在肾脏中的代谢是通过一系列步骤和途径完成的,而每一步所占的比重又各不相同,其中全部尿酸都经过肾小球滤过,绝大部分 在肾小管重吸收,半数尿酸在肾小管再分泌,40%在分泌后进行再次重吸收。最后只有8%~12%的尿酸通过肾小球滤过随尿液排出体外。
一旦这几个步骤没有完成其预期效果或者是受到一些外界因素影响如高血压、药物、细胞外液量、有机酸增多性疾病时,就会影响肾脏对尿酸的排泄。
二、高尿酸血症肾脏损害的发生机制
近期,关于高尿酸血症肾脏损害的发生机制研究已经受到肾脏病学者的广泛关注。其发生机制主要包括高尿酸血症的直接损伤和间接损伤引起肾脏结构和功能改变,导致终末期肾脏疾病的发生。
目前,高尿酸血症肾脏损害机制研究热点主要集中在高尿酸血症的间接损伤,包括血尿酸增高对血管内皮的损伤、高尿酸导致肾素-血管紧张素-醛固酮系统激 活、高尿酸血症刺激炎性反应级联反应、高尿酸血症导致机体代谢综合征发生、高尿酸血症引起肾脏肾小管上皮细胞转分化为肾间质成纤维细胞等,加重慢性肾脏病 进展。
(一)高尿酸血症的直接损伤
由于原发性或继发性高尿酸血症使体内的血尿酸浓度异常增高,当体液pH值为7.4时,绝大多数尿酸(超过95%)在血浆,肾小球滤过液和肾间质中将解离成尿酸盐离子。
在pH值、逆流倍增机制和高浓度尿酸盐离子(大于500μmol/L)的共同作用下,尿酸转换为单盐-水化合物或尿酸盐结晶,并大量沉积在肾小管和肾间质中,造成肾脏的实质性损害,如炎性反应和纤维化的形成。
同时高尿酸血症形成的尿酸结石对肾脏的直接损伤就是梗阻,以及梗阻引发的一系列如感染、出血、积水、恶性变等并发症。
(二)高尿酸血症的间接损伤
通过腺嘌呤法、酵母法促进尿酸生成增多,或是抑制尿酸排泄,以及基因重组法建立高尿酸血症大鼠模型,研究证实这一类高尿酸血症大鼠更易发生肾脏肥大、 蛋白尿、间质纤维化、肾小球硬化症、人球小动脉病变等同时,研究发现高尿酸血症加重肾脏损伤是通过多种机制共同实现的,包括RAS系统的激活、炎性反应、 肾小管上皮细胞转分化、促进血管平滑肌细胞和血管内皮细胞的增殖、血液粘稠度增加和代谢异常等。
1.高尿酸血症与血管病变:
在血管平滑肌细胞上存在的尿酸盐转运通道(URAT1)对丙磺舒特异性敏感,尿酸通过此阴离子通道进人血管平滑肌细胞后,首先接触并激活的是MAPK通路,刺激特异性的丝裂原活化蛋白激酶,导致C0X-2高表达,并上调血小板源性生长因子促进血管平滑肌细胞的增殖。
研究显示,在高尿酸血症患者的肾脏组织中检测到单核细胞趋化蛋白l(MCP-l)的表达量高于正常值,也同样导致血管平滑肌细胞增殖、巨噬细胞浸润,加重肾脏损害。
在一项动物实验研究中,研究者给高尿酸血症大鼠口服别嘌醇或苯溴马龙来降低其血尿酸水平,提高NO水平,最终结果可明显逆转血压的升高和减轻肾功能损 伤。从而证明NO对于血管内皮细胞有保护作用,而血尿酸水平与NO降低以及血管内皮细胞损伤程度这三者之间呈线性相关。
进而有学者在研究尿酸对血管内皮细胞作用机制中,发现人体内的尿酸和NO水平存在着动态平衡关系。由于尿酸有作为抗氧化剂的能力,所以异常增高的尿酸会和NO产生氧化还原反应,导致对人体有益的NO被大量的消耗。
因此高尿酸血症患者体内的高尿酸水平可以通过多种途径降低内皮细胞的NO水平,导致血管内皮细胞功能异常,血管舒张作用减弱,进而引起高血压和血管病变。
此外,尿酸导致的血管病变还表现在尿酸可增加血液粘稠度。由于尿酸属于弱酸,在血浆中无法完全溶解,不能溶解的尿酸以尿酸单盐的形式存在。
一旦PH或者温度发生改变时,这部分的单盐就可转换为无定形的尿酸钠微小结晶。这些细小的沉淀可使血浆粘稠度增加,提高了血栓形成的风险,引起肾脏损害。
2.高尿酸血症与RAS:
在国外的一项研究中发现,在CKD患者中,使用别嘌呤醇治疗高尿酸血症后,可使血压明显下降,并在一定程度上抑制了肾功能的进展。而当别嘌呤醇的治疗停止后,研究人员观察到患者的血压又持上升趋势,且肾脏损害进一步加重。
并且这一现象只能在那些没有事先接受血管紧张素转换酶抑制剂(ACEI)或血管紧张素受体阻滞剂(ARB)的患者中出现,从而证明肾素-血管紧张素系统(RAS)在高尿酸血症对高血压和肾脏损害的影响机制中起重要作用。
异常激活的RAS系统和肾小球内的“三高”现象共同降低了肾小管内皮细胞的功能,引发肾脏损伤,并最终发展为肾衰竭等终末病变。
3.高尿酸血症与炎性反应:
在尿酸通过炎性反应级联反应导致尿酸性肾病的发生机制中,Toll样受体(TLRs)在其中发挥了重要作用。最近的研究发现,TLRs能识别尿酸结晶释放的被称为“危险信号(DAMPs)”的蛋白质成分。
一部分尿酸钠结晶直接识别并激活TLRs,其余则通过信号通路间接激活TLRs,且需要结合素、Cm6、Fc受体或CD14的参与,最终激活NF-kB。而NF-kβ又参与了MyD88依赖性途径的活化和转位,完成炎性反应的信号转导过程。
并在此过程中激发了特定基因序列的表达和炎性因子的生成,如肿瘤坏死因子α(TNF-α)和白细胞介素l(IL-l),从而介导痛风性关节炎和高尿酸 肾损害的发生。Liu-Bryan等在急性痛风性炎性反应的小鼠模型中,对做了基因敲除的TLR-2-/-、TLR-4-/-、MyD88-/-的同基因 型的小鼠注射了尿酸钠结晶。
结果证实,无论体内还是体外实验,都发现炎性因子的表达受到了显著的抑制,即TLRs参与的炎性反应在这些小鼠模型中没有得到体现。
尿酸介导的血管炎性反应是高尿酸肾损害的另一重要机制。在血管平滑肌细胞中,血尿酸刺激诱导血管平滑肌的增殖,同时还可上调C反应蛋白和单核细胞趋化蛋白1的表达来促进炎性反应的发生,引起血管内皮功能的损伤,从而加重肾脏损害。
4.高尿酸血症与代谢综合征:
代谢综合征(metabolicsyndrome,MS)是一组临床症候群,他不是单一疾病引起的,而是一系列相关疾病的共同结果,如高血糖、胰岛素抵抗、肥胖、血脂异常、高血压等,并严重影响人类健康。
而很多研究也证实了,高尿酸血症与代谢综合征的众多病因如高血糖、肥胖、血脂异常、高血压以及胰岛素抵抗有一定关联。我们课题组蒋茜等,应用腺嘌呤 (0.1g.kg-1.d-1)联合氧嗪酸钾(1.5g.kg-1.d-1)混悬液每日早晚两次灌胃给药,成功建立大鼠高尿酸肾病动物模型,发现高尿酸肾 病大鼠血脂明显升高。
虽然高尿酸血症导致的代谢综合征没有产生实质性的肾脏疾病,但不可否认的是MS中的高血脂、高血压、高血糖都会加重肾脏的负担以及CKD的进展。
同时高尿酸血症和代谢综合征之间存在着恶性循环的关系,彼此都会加重对方的危害程度。如研究表明,高血压,特别是收缩压对高尿酸血症的影响较大。
在胰岛素抵抗的研究中,也证实了中心性肥胖者常合并有一定程度的胰岛素抵抗,导致高胰岛素血症,胰岛素不仅干扰脂质代谢,加重血脂代谢紊乱,还可促进肾小管对尿酸的重吸收,从而加重高尿酸血症。
5.高尿酸血症与肾小管上皮细胞转分化:
肾小管上皮细胞表型转化、α平滑肌肌动蛋白(α-smoothmuscleactin,ot-SMA)表达、大量细胞外基质成分产生、在肾脏间质堆积是肾间质纤维化的重要发生机制。
研究显示,高尿酸血症肾损害大鼠模型中,a-SMA表达显著上调,E-cadherin蛋白表达显著下调;别嘌醇处理的尿酸性肾病大鼠,肾小管上皮细 胞转分化标志物α-SMA表达显著下调,E-cadherin蛋白表达下调;在体外培养的肾小管上皮细胞中,尿酸刺激肾小管上皮细胞转分化,尿酸转运蛋白 抑制剂可抑制尿酸刺激的肾小管上皮细胞转分化。证实高尿酸血症可能通过诱导肾小管上皮细胞表型转化,促进肾间质纤维化的进展。
三、小结与展望
综上所述,高尿酸血症肾脏损害包括血尿酸增高所致的直接损伤和间接损伤两类发生机制。直接损伤即机械性损伤是高尿酸血症导致集合管肾间质尿酸盐结晶形 成所致的肾脏损伤;间接损伤是指高尿酸血症通过促进细胞表型转化、炎性反应级联反应、RAS系统的激活、抑制NO的表达、促进血管平滑肌细胞增殖等作用导 致肾脏病变;反之肾脏病变降低了尿酸的排泄率,血尿酸水平进一步升高。
两种机制对肾脏产生的损害,致使肾小球滤过率下降,并最终导致肾脏纤维化和肾衰竭,同时随着肾脏疾病的进展会导致血尿酸进一步的升高,二者互相促进。
高尿酸血症是多基因参与的遗传性疾病,高尿酸血症对肾脏的损害也由多种机制共同参与,其中一些具体致病机制尚未完全研究清楚,且尿酸增多的机制受环境因素影响较大,其发病因素众多,又与多种疾病关系密切,很多方面都有待进一步的研究。
在今后的研究中,应着重于基因分析、代谢通路与环境因素相结合,并在临床病例中多实践和运用计算机信息技术的分析能力,这些可能会成为该疾病研究的发展趋势。
中华肾脏病杂志2014年10月第30卷第10期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








非布司他降尿酸蛮好的
143
轻度肾脏疾病对母亲和婴儿可能会增加孕期风险
152
好文章,超赞
102
愈来愈重视
133
#研究进展#
36
#高尿酸#
36
bad something !
139
痛风其中之一
43