SCI REP:中性粒细胞与淋巴细胞比值基础值与变化值对肿瘤患者预后的影响!
2017-04-09 xing.T MedSci原创
总之,基础NLR和ΔNLR是接受化疗的晚期胰腺癌患者患者的独立预后预测因素。
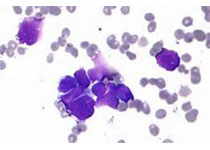
胰腺癌是美国男性和女性中因肿瘤死亡的第四大死因。一般而言,诊断为晚期胰腺癌患者的治疗方案较为有限。患者的5年生存率也低于5%。中性粒细胞-淋巴细胞比值(NLR)已被证实与多种肿瘤的预后相关。近日,Scientific reports 杂志上发表了一篇研究文章,研究人员旨在评估接受化疗的晚期胰腺癌患者基础NLR和NLR变化值(ΔNLR)的预后作用。
在2010年1月至2015年6月期间,132名接受化疗的患者符合评估条件。基于该研究中患者的数据,根据接受者操作特征曲线NLR的临界值为2.78。研究人员观察到高水平的基础NLR(NLR>2.78)对总体生存而言是一个不良预后因素(多变量风险比为2.648,P<0.001)。进行2个周期的化疗后增加的NLR(ΔNLR>0)与更高的不良预后风险相关,相比于ΔNLR≤0的患者(多变量风险比为1.894,P=0.007)。结合NLR和ΔNLR因素,多因素分析显示2个周期的化疗后高基础NLR和增加的NLR患者风险显著增加(风险比为5.817,P<0.001),相比于基础NLR较低和ΔNLR<0的患者。
总之,基础NLR和ΔNLR是接受化疗的晚期胰腺癌患者患者的独立预后预测因素。
原始出处:
Yang Chen, et al. Significance of baseline and change in neutrophil-to-lymphocyte ratio in predicting prognosis: a retrospective analysis in advanced pancreatic ductal adenocarcinoma. Scientific reports. 2017. http://www.nature.com/articles/s41598-017-00859-5
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#患者预后#
52
#中性粒细胞#
62
#淋巴细胞#
0
#肿瘤患者#
69
确实如此 这也是反应了免疫对肿瘤的反应~
84
涨知识了
73
学习了,谢谢
64
对临床实用值得共享
68
好好学习,涨知识
74
目前炎症指标与肿瘤预后是研究热点
51