J Arthroplasty:TKA中使用含抗生素骨水泥不会影响细菌感染谱、耐药谱
2014-08-26 jianmolanyin 丁香园
目前美国只有6种不同类型的含抗生素骨水泥且只能用于分期关节置换术的第二阶段,在初次关节置换术中预防应用含抗生素骨水泥尚未被认可,1995年的调查数据显示只有10%-13%的美国骨科医生在初次THA 或TKA中经常性使用抗生素,但为了预防假体周围感染、降低致残致死率以及减少与之相关的医疗花费,越来越多的美国外科医生在初次膝关节置换术中加入低剂量的抗生素。 从理论上分析预防性应用含抗生素
目前美国只有6种不同类型的含抗生素骨水泥且只能用于分期关节置换术的第二阶段,在初次关节置换术中预防应用含抗生素骨水泥尚未被认可,1995年的调查数据显示只有10%-13%的美国骨科医生在初次THA 或TKA中经常性使用抗生素,但为了预防假体周围感染、降低致残致死率以及减少与之相关的医疗花费,越来越多的美国外科医生在初次膝关节置换术中加入低剂量的抗生素。
从理论上分析预防性应用含抗生素骨水泥的收益可能大于潜在的副作用,大量文献也证明了这点,但是反对者认为在初次关节置换中预防性应用抗生素可能导致潜在的风险,比如增加了花费、影响到了骨水泥的机械特性、全身性的毒性反应、过敏反应以及细菌耐药等。Erik N. Hansen等人对此进行了研究,研究假设假设在全膝关节置换术患者预防性应用素的骨水泥不会显著影响到病原体的耐药谱,最终的结果发表于近期的The Journal of Arthroplasty上。
该回顾性队列研究获得了作者所在单位的审查委员会(institutional review board IRB)的批准,所纳入的患者是运用“假体周围感染”(PJI)等合适的检索词从作者所在研究机构的数据库筛选并确认的,均为2000年1月1日至2009年那12月31日因全髋或全膝置换术后假体周围感染而接受治疗的病例,这些患者在该时间段内在作者的工作单位行初次关节置换术,并且记录了骨水泥的使用情况。
研究阶段内(2000年至2009年除外2003年,因为2003起该研究中心的外科医师开始广泛应用含抗生素的骨水泥,所有在2003年行THA或TKA的患者均排除在本研究之外。),共有11,469名患者行初次全髋关节置换术及11,494例行全膝关节置换术,总体上来说假体周围感染(PJI)的发生率是逐年降低的:在2003年前全膝置换患者的PJI发生率为2% (61/3,053);2003年以后该数据为0.7% (59/8,441, P = 0.0001),差异有统计学意义;与此对比的是在2003年前全髋置换患者的PJI发生率为0.6% (21/3,352)。2003年以后该数据为0.4% (33/8,117, P = 0.16),差异无统计学意义。
研究中共有174例患者(男86例,女88例,平均64岁;120例患者涉及膝,54例涉及髋)关节置换术后出现了假体周围感染,此类患者根据手术类型和时间共分为四组:1组为TKA非抗生素骨水泥组(非ALBC 组,2003年前的TKA,n = 61/3,053, 2%);2组为TKA含抗生素骨水泥组(含ALBC 组,2003年后的TKA,n = 59/8,441, 0.7%);3组为2003年前行THA手术的患者(对照组, n = 21/3,352, 0.6%);4组为2003年后行THA手术的患者(对照组,n = 33/8,117,0.4%)。
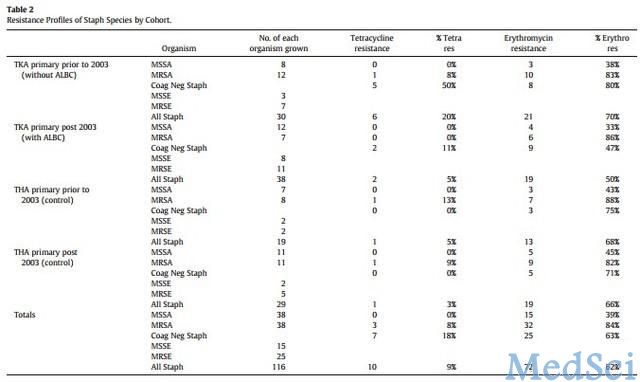
174例患者,其中143例 (82%)细菌培养为阳性,某些培养结果为混合性感染,大约三分之二的患者为金葡菌或者凝固酶阴性的金葡菌感染(116例,约67%患者为金葡菌培养阳性),感染病原菌额情况见见表一。除金葡菌外,其他最常见的病原菌包括肠球菌属、假单胞菌属等,比如B组链球菌(9例),粪肠球菌(8例)。由于金葡菌及凝固酶阴性的金葡菌是最具代表性的病原菌,本研究着重对着两种病原菌的耐药模式进行了分析,其中金葡菌对对甲氧西林,红霉素和四环素的耐药比重详见表二。
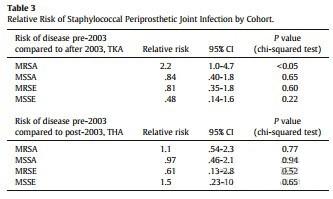
此外金葡菌对甲氧西林的耐药率显著下降,由40%降为 18%(P= 0.048),但表皮葡萄球菌对甲氧西林的耐药率有所增加,由23%增为 29%,(p =0.6),差异无统计学意义。与此不同的是耐甲氧西林的金葡菌的感染率在应用含骨水泥的抗生素后(2003年后)是未应用时的2倍(优势比2.2, 95%可信区间 1.0–4.7,P<0.05,详见表三),其他类型的金葡菌导致的假体周围感染耐药率差异无显著意义,在同一阶段所有金葡菌病原体对四环素的耐药率由20%降为 5% ,对红霉素的耐药率由70%降为50%,但差异均无显著意义(P=0.14,p = 0.43)。
表一:研究中出现的病原微生物感染情况
表二:研究中金葡菌耐药情况
表三:2003年前后假体周围金葡菌感染相对风险
由于本文为回顾性研究,不可避免的存在某些局限及猜测;所涉及的样本量较少;某些感染患者在其他医疗机构进行了治疗但研究者并没有了解到这些情况;方法学上本文并非随机对照研究,而是采取的队列研究—未采用含抗生素骨水泥的关节置换患者(如全髋关节置换患者)作为对照组以发现任何感染菌耐药模式的变化,尽管如此仍有很多混杂因子无法控制甚至影响到研究结果(比如患者的并发症等),因此作者并没有给予肯定的结论,仍需进一步研究来证实。
但研究者们坚信本文的结论仍具有价值—至少反应了北美一家关节置换手术量较大的医疗机构的最少5年随访的经验,未来作者计划寻求多个医疗机构的合作以获得足够的样本从而使得结果在统计学上更具有意义。最后作者认为为进一步降低假体周围感染的发生率,关键是阐明诸如含抗生素的骨水泥等内植物如何对假体局部微生物产生最终的影响。
原始出处:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AST#
64
#细菌感染#
0
#ART#
85
#骨水泥#
92
#TKA#
75