Heart:复发性心内膜炎的临床特征和结局
2022-06-03 MedSci原创 MedSci原创
复发性和首发性IE患者的住院和1年死亡率相似,但预后不良的预测因素相似。
感染性心内膜炎(IE)仍然是高发病率和死亡率的负担,尽管诊断和治疗策略有所改进。最近研究的结果表明,IE患者通常有多种合并症,当有必要时不进行手术与较差的结局相关。

近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究的目的是比较复发性和首发性心内膜炎(IE)患者的临床病程和结局。在欧洲心内膜炎(EURO-ENDO)的156个中心登记的复发性和首发IE患者中,研究人员采用倾向评分匹配法进行了比较。复发性IE分为在前一次发作后≤6个月发生的复发性IE或在前一次发作后6个月以上发生的再感染。

该研究共纳入了3106例患者,其中首发IE患者2839例(91.4%),平均年龄为59.4(±18.1)岁;复发性IE患者267例(8.6%)(平均年龄为58.1(±17.7)岁;74.9%为男性)。在复发性IE患者中,13.2%的患者为静脉吸毒者(IVDUs), 66.4%的患者进行了三尖瓣瓣膜修复或更换,而且较首发IE患者更易受损伤(20.3% vs 14.1%;p=0.012)。
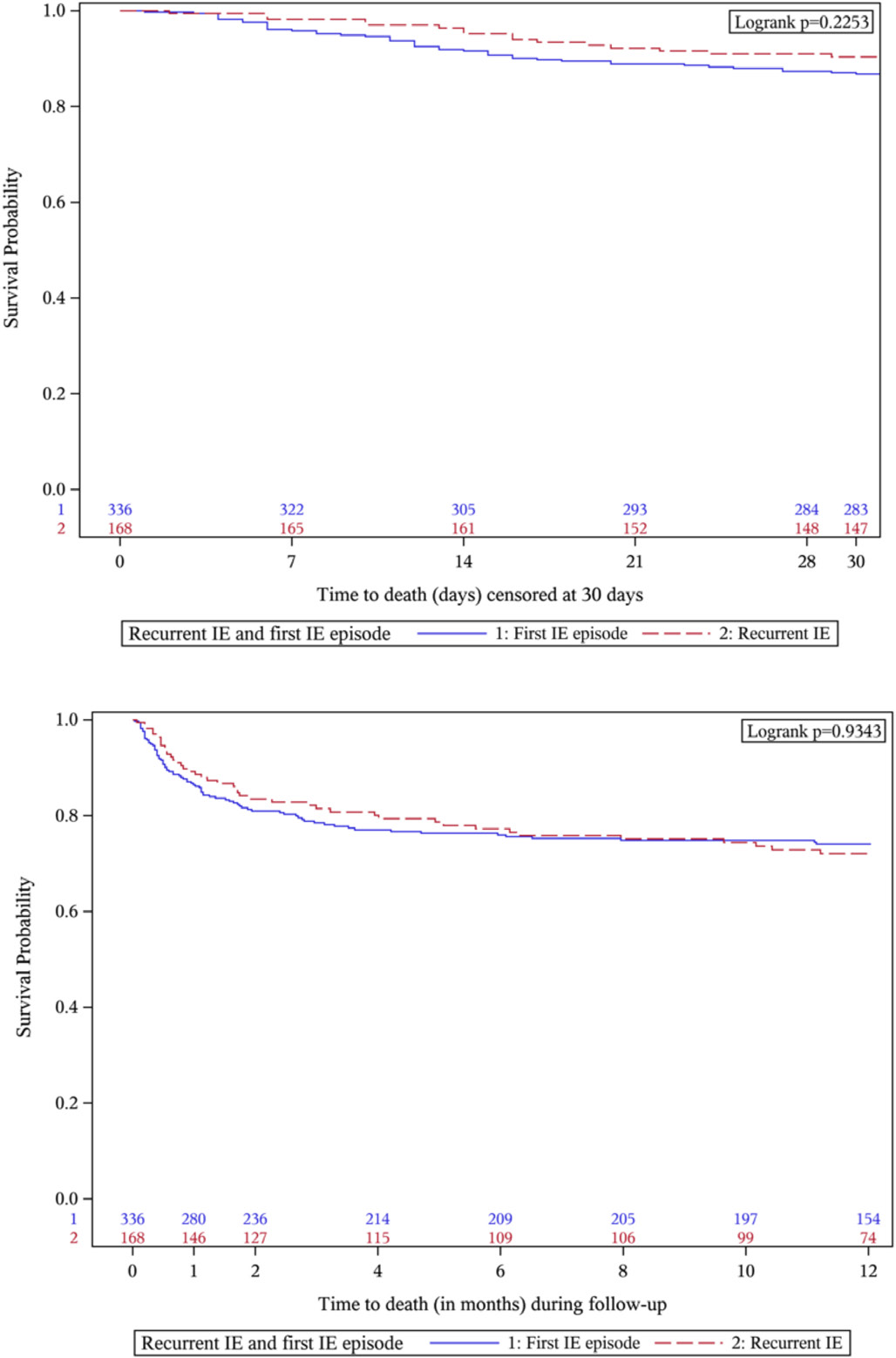
在首发IE患者中,主动脉瓣受累率较高(45.6% vs 39.5%;p = 0.061)。复发和再感染分别为20.6%和79.4%。金黄色葡萄球菌是两组患者中最常见的微生物(p=0.207)。复发性和首发性IE患者的住院和住院后死亡率没有差异。在复发性IE患者中,IVDU患者的住院死亡率较高。包括心源性和感染性休克的发生、瓣膜病的严重程度和有手术指证而未进行手术在内的较差住院和1年结局的独立预测因素在复发性IE和首发IE患者中相似。
由此可见,复发性和首发性IE患者的住院和1年死亡率相似,但预后不良的预测因素相似。
原始出处:
Rodolfo Citro.et al.Clinical profile and outcome of recurrent infective endocarditis.heart.2022.https://heart.bmj.com/content/early/2022/05/30/heartjnl-2021-320652
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#临床特征#
0
#复发性#
71
#内膜#
59
学习了
66
#心内膜炎#
120
#ART#
44
#HEART#
0
学习了#学习#
67
了解一下
67