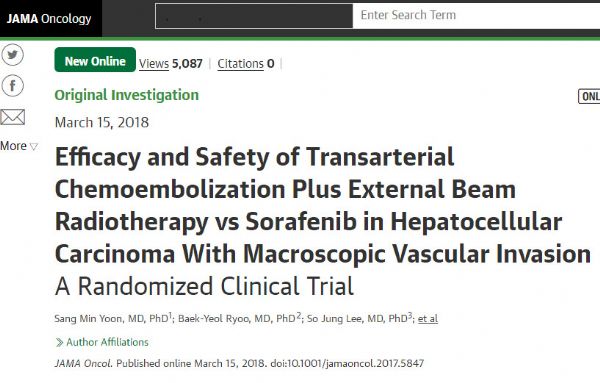
Radiology:肝癌都这么大了,如何治疗才能提高生存期呢?
2018-05-21 shaosai MedSci原创
本研究旨在验证索拉菲尼联合经动脉化学栓塞(TACE)和射频消融(RFA)(S-TACE-RFA)治疗中或大肝细胞肝癌(HCC)的安全性和疗效,并将结果发表在Radiology上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了,谢谢分享
82
学习了
99
谢谢分享
90
学习了学习了
96
好知识值得借鉴!
92
#生存期#
30
学习了
32
阅
54
学习
45
不错的方法
36