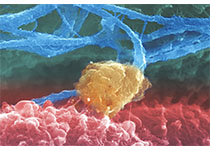
肿瘤合并心脏病的多角度整合防治策略
2018-01-21 夏云龙 吕海辰 医师报
当今世界,医疗科技的飞速发展使得恶性肿瘤不再是不治之症,越来越多的肿瘤患者在经过合理治疗后长期生存,很多类型的肿瘤以一种慢性病的形式长期存在。基于此,大量肿瘤幸存者死于非肿瘤原因,其中以心血管疾病尤为常见。另一方面,随着新技术、新疗法的爆发式涌现,现代医学也渐进式地呈现出了专科化、专业化发展的划分格局。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了.了解.了解
92
肿瘤合并心脏病治疗原则应根据临床情况区别对待.
91
学习了新知识
84
学习谢谢分享
0
谢谢分享.学习了
98
了解了解.继续关注
66
学习了.谢谢
51
双心治疗呗!
50
^_^^_^
49
好好学习天天向上
53