JNNP:弓亨特综合征:一例双侧椎动脉动态闭塞的罕见病例
2021-06-20 MedSci原创 MedSci原创
一位54岁的男子,主诉偶发耳鸣和视力模糊2年 多年来,尤其是开车时,症状与右转头部有关。神经学检查突出了报告的症状出现在颈部右侧扭转超过45° 。在初步的彩色多普勒超声检查后,病
一位54岁的男子,主诉偶发耳鸣和视力模糊2年 多年来,尤其是开车时,症状与右转头部有关。神经学检查突出了报告的症状出现在颈部右侧扭转超过45° 。在初步的彩色多普勒超声检查后,病人接受了主动脉上干的动态增强磁共振血管成像(CE-MRA)。中立位椎动脉血流及口径规则,无明显优势;头部右转超过60度时进行了扫描° 显示双侧血管动态狭窄,尤其是右侧C5–C6水平和左侧C2水平。
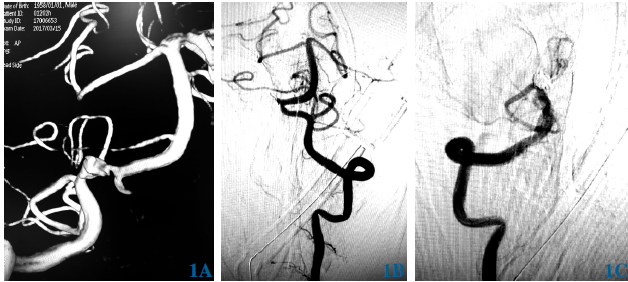
在右头旋转期间进行的动态CE-MRA扫描显示右侧C5–C6水平(A,白色箭头)和左侧C2水平(B,黑色箭头)的椎动脉双侧狭窄。增强磁共振血管成像。为了确诊,我们进行了动态数字减影血管造影(dDSA),并在不同程度的右颈部旋转时选择性地注射VAs。dDSA证实了CE-MRA的发现,诊断为双侧血管动力性狭窄的弓亨特综合征(BHS)。
dDSA图像显示正常的左心室内径和中性位置的血流(a)在右脑旋转期间(B),观察到由于C2水平的动态狭窄(黑色箭头)导致血流中断(白色箭头)。注意在同一水平(黑色箭头)颈升动脉对血管的再灌注。动态数字减影血管造影。检查还显示存在一个单一的薄后交通动脉,进一步解释了代偿流量不足。为完成诊断而进行的CT扫描突出了该综合征潜在的可能的器质性改变。检查显示右C5横孔的口径减小,这是由于近中骨赘骨刺可能对血管有压迫作用
BHS是一种罕见的神经血管疾病,其特征是VA的动态闭塞和头部旋转引起的后脑循环血流不足。症状学依赖于代偿性血流,范围从短暂的头晕、晕厥、眼球震颤、耳鸣到血栓栓塞并发症。在大多数情况下,VA的动态闭塞是由于血管过程中的外源性压迫所致,而在中立位时血流无明显改变;这种压迫作用是由颈部旋转引起的。寰枢椎关节是椎动脉的主要薄弱点,这是由于椎动脉在横孔处的生理性低活动性所致。在对侧颈旋转时,这种情况易导致寰枢椎韧带下或C1和C2孔之间的血管变薄或闭塞。因此,该综合征通常发生在这个水平(寰枢椎BHS),很少发生在亚轴型和混合型BHS。后者是一种罕见的情况,影响我们的患者。包括双侧椎动脉狭窄,一个位于C1/C2,另一个位于轴下。此外,BHS的动态闭塞通常影响显性VA,而非显性对侧VA由于发育不全、狭窄或解剖造成的血流补偿不足。如我们所描述的,很少有病例报告BHS伴有非显性VA6的孤立性动态闭塞,甚至更少的BHS伴有无VA显性的双侧动态闭塞。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#罕见病例#
83
#综合征#
56
#罕见#
70
#双侧#
83