Circulation:桡动脉血管作为补充移植物可降低不良心血管事件的发生风险!
2017-06-01 MedSci MedSci原创
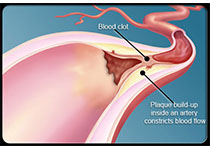
桡动脉(RA)血管是否可以改善冠状动脉旁路移植(CABG)手术的临床疗效? 近日在circulation上发表的一篇文章针对该点展开研究。该研究建立了动态血运重建试验(ART),这项试验旨在评估双侧内胸动脉(BITA)在单个左内胸动脉(SITA)上的存活率情况。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#植物#
73
#血管事件#
76
#动脉血#
72
#桡动脉#
79
#移植物#
91