J Cell Physiol:弥漫性低级胶质瘤的肿瘤微环境中的免疫相关基因和免疫细胞浸润的研究报告
2020-05-26 MedSci原创 MedSci原创
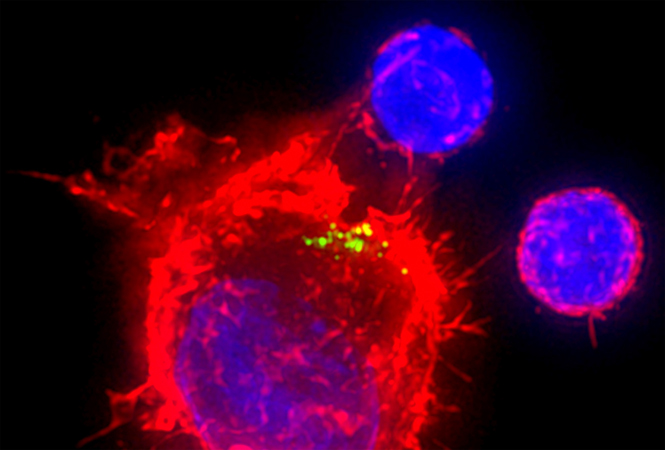
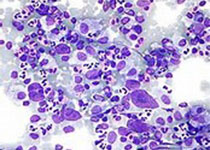
肿瘤微环境与肿瘤的发生、进展和预后高度相关。本研究旨在探究低级胶质瘤(LGG)肿瘤微环境中免疫相关基因(IRG)的表达和免疫浸润模式。
肿瘤微环境与肿瘤的发生、进展和预后高度相关。本研究旨在探究低级胶质瘤(LGG)肿瘤微环境中免疫相关基因(IRG)的表达和免疫浸润模式。
我们使用表达数据(ESTIMATE)算法对恶性肿瘤组织中的基质细胞和免疫细胞进行了估算,以基于癌症基因组图谱数据集计算免疫和基质评分并确定预后的IRG。在功能富集分析和蛋白-蛋白相互作用网络的帮助下,探讨了这些基因的潜在分子功能。值得注意的是,从中国胶质瘤基因组图谱数据库中下载的3个队列分析,进一步验证了这些基因的预后价值。此外,利用肿瘤IMmune估算资源(TIMER)算法估算了浸润免疫细胞的丰度,探索了LGG的免疫浸润模式。无监督聚类分析确定了三个免疫浸润模式的聚类,并表明CD8+ T细胞和巨噬细胞与LGG的结果显著相关。
总的来说,我们的研究确定了一系列预后性的IRG,为探讨LGG的免疫浸润模式提供了一个视角。
原始出处:
Xiangyang Deng, Dongdong Lin, et al., Profiles of Immune-Related Genes and Immune Cell Infiltration in the Tumor Microenvironment of Diffuse Lower-Grade Gliomas. J Cell Physiol. 2020 Mar 11. doi: 10.1002/jcp.29633.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
49
#Cell#
54
#Physio#
69
#相关基因#
58
#研究报告#
43
#弥漫性#
47