ONC201治疗胶质瘤的I / II期临床研究即将在日本开展
2020-04-02 Allan MedSci原创
Oncoceutics制药公司宣布,ONC201已在临床前模型和多项正在进行的临床试验中证明了其抗胶质瘤的有效性和安全性。
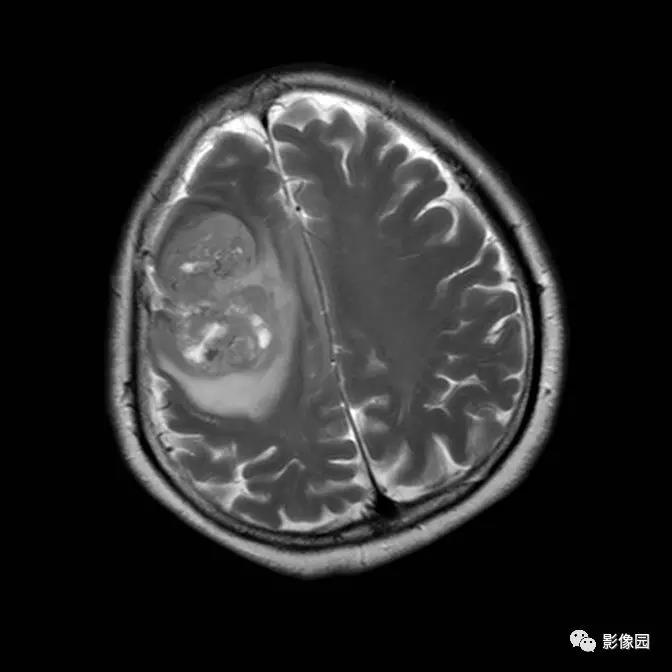
Oncoceutics制药公司宣布,ONC201已在临床前模型和多项正在进行的临床试验中证明了其抗胶质瘤的有效性和安全性。ONC201是一种多巴胺受体D2(DRD2)的高度选择性拮抗剂,能够有效穿透血脑屏障。ONC201的DRD2拮抗作用与经过验证的抗癌途径有关,可导致癌细胞凋亡。Oncoceutics已使用ONC201在实体瘤中成功完成了一项I期临床研究,并且正在进行其他针对实体和血液恶性肿瘤的I / II和II期临床计划。
Oncoceutics首席运营官Lee Schalop表示:“随着我们将ONC201的开发范围扩展到美国以外的重要市场,ONC201将为日本神经胶质瘤患者提供一种新的治疗选择”。胶质瘤占脑实质内原发性肿瘤的绝大多数。胶质瘤是指组织学特征与正常胶质细胞(即星形胶质细胞、少突胶质细胞和室管膜细胞)相似的肿瘤。每种胶质瘤的生物学侵袭性都存在很大的变化范围。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#I期临床#
0
#II期临床研究#
69
期待国内有临床计划
136
#日本#
73
#II期临床#
75