Exp Hematol:血清 B 细胞成熟抗原是未经治疗的慢性淋巴细胞白血病的独立预后标志物
2022-06-03 网络 网络
sBCMA升高强烈提示CLL活跃,在CLL-IPI和IPS-E评分中增加sBCMA的测量,可以提高其预测新诊断患者预后的能力
慢性淋巴细胞白血病(CLL)是一种单克隆B淋巴细胞的淋巴增生性肿瘤,累及外周血、骨髓和淋巴器官。CLL国际预后指数(CLL-IPI)和早期国际预后评分CLL (IPS-E)是临床上常用的指导治疗和预测预后的评分,但这两个评分都不能准确预测早期CLL的病程,也不能明确指定何时开始治疗。
于是,一个简单的、非侵入性的检测来识别一个高表达的、敏感的、与疾病活动相关且不与其他因素(如肾损害)混淆的生物标志物是理想的。B 细胞成熟抗原 (BCMA) 是一种在成熟 B 淋巴细胞上表达的细胞膜受体,在包括慢性淋巴细胞性白血病 (CLL) 在内的 B 细胞恶性肿瘤患者中发现其血清水平升高。因此,一研究团队认为作为肿瘤坏死因子受体(TNFR)超家族成员之一的b细胞成熟抗原(BCMA)的血清水平将是评估CLL临床预后的一个有价值的生物标志物。
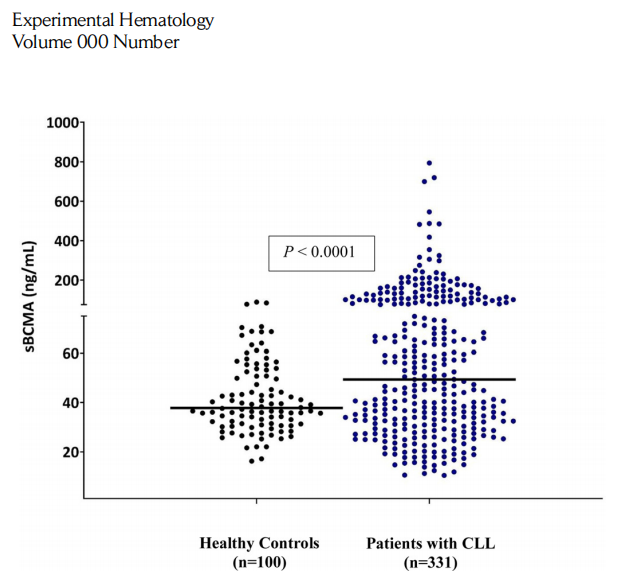
图1:健康对照组与慢性淋巴细胞白血病(sBCMA)患者的血清b细胞成熟抗原(CLL)患者。对331例未经治疗的新诊断的CLL患者的样本进行检测,发现中位sBCMA为48.6ng/mL。100名年龄和性别匹配的健康患者的对照组样本产生的sBCMA中位数为37.8ng/mL。与对照组相比,CLL患者的血清BCMA水平显著升高(p<0.001)。
研究人员使用酶联免疫吸附试验和多克隆抗 BCMA 抗体测量了 331 名未经治疗的新诊断 CLL 患者的血清 BCMA (sBCMA) 水平。与年龄和性别匹配的健康对照以及基于预后因素的更活跃的 CLL 患者相比,研究人员发现CLL 患者的 sBCMA 水平升高。他们使用 Mann-Whitney 和 Kruskal-Wallis 检验比较了 sBCMA、首次治疗时间 (TTFT)、总生存期 (OS) 和多种预后因素之间的关系。
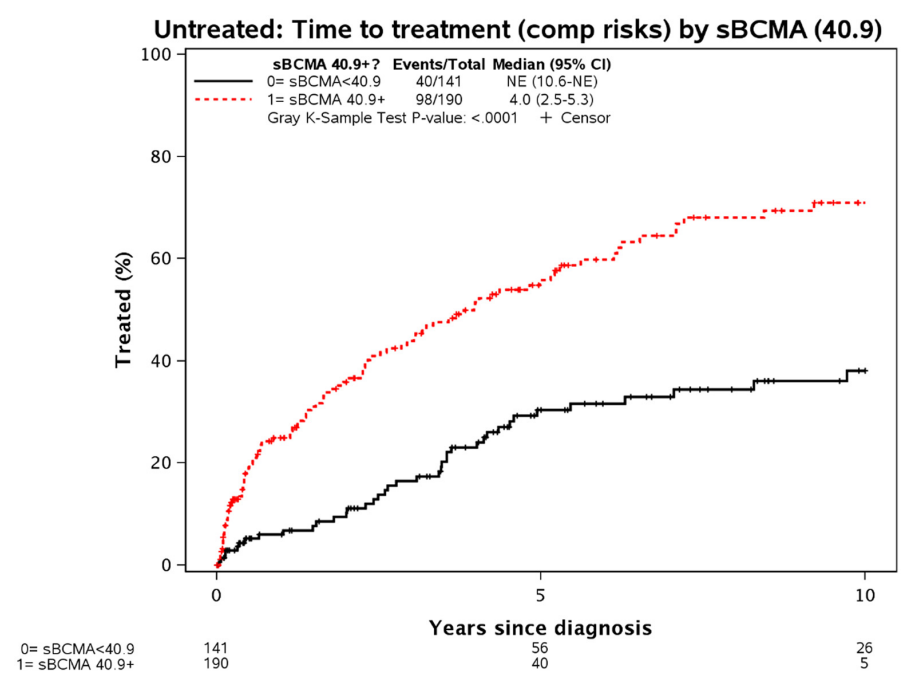
图2:基于血清b细胞成熟抗原(sBCMA)水平高于或低于40.9ng/mL的最佳临界值的慢性淋巴细胞白血病(CLL)患者的首次治疗时间。
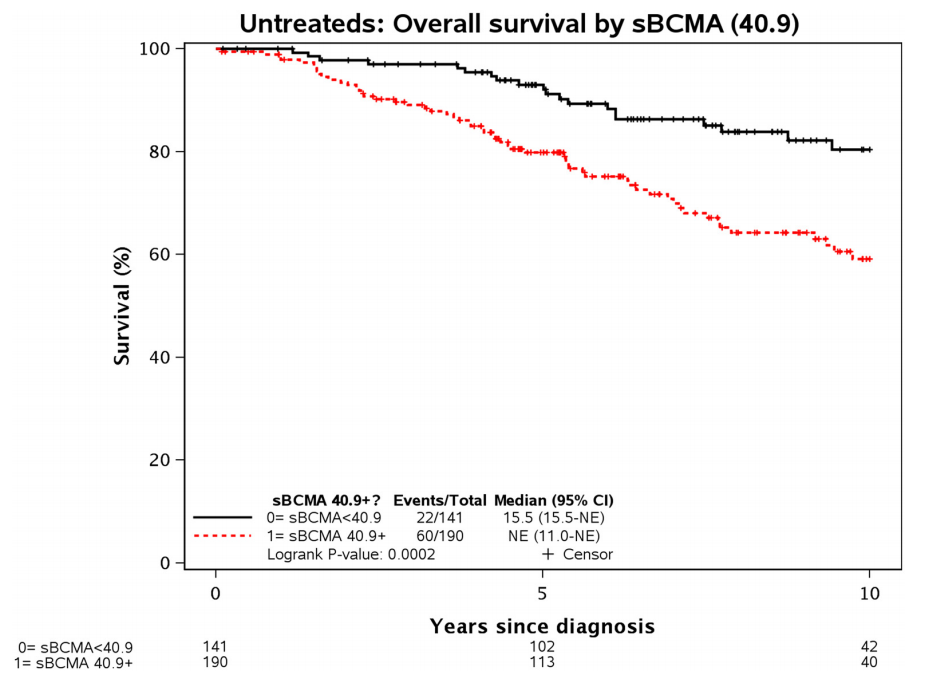
图3:基于血清b细胞成熟抗原(sBCMA)水平高于或低于40.9ng/mL的最佳临界值的慢性淋巴细胞白血病(CLL)患者的总生存期。
与年龄和性别匹配的健康受试者 (n = 100; 37.8 ng/mL) 进行比较,CLL 队列的中位 sBCMA 水平 (48.6 ng/mL) 显着更高 (p < 0. 001) 。血清 BCMA 与 TTFT([HR] = 2.9,95%CI 2.0-4.2,p < 0.001)和 OS(HR = 2.5,95%CI 1.5-4.0,p < 0.001)相关。
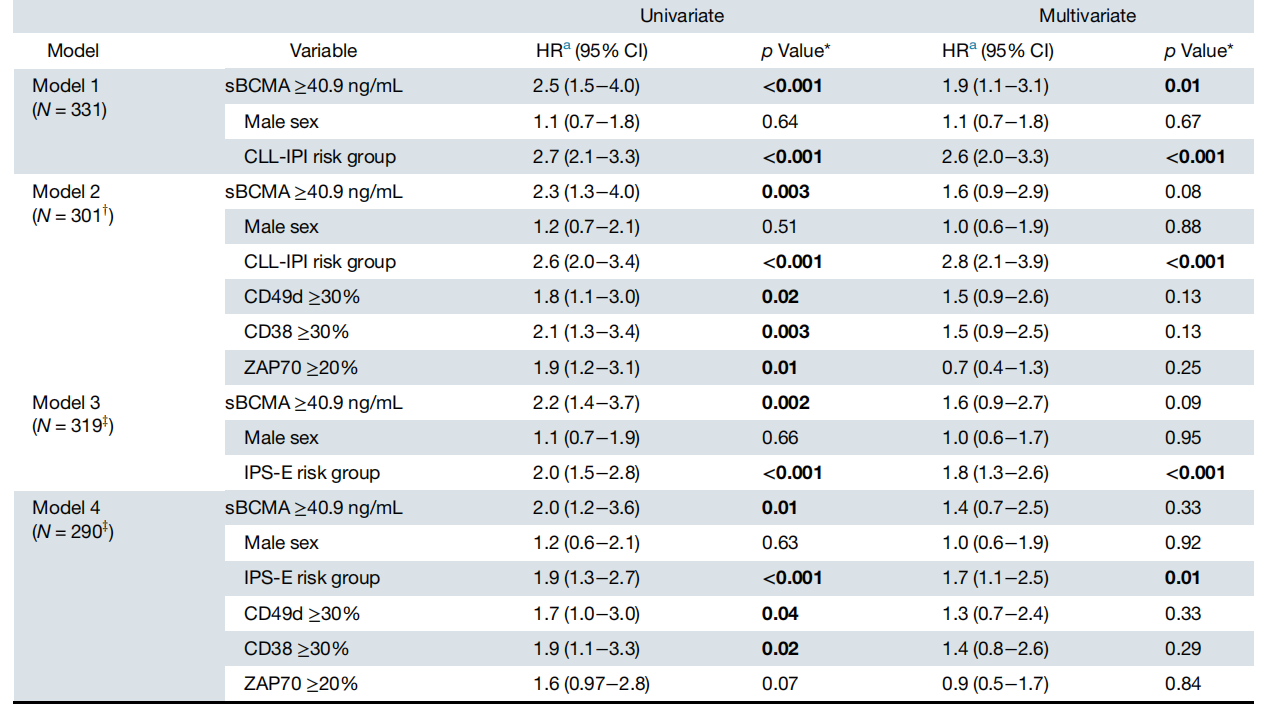
表:总生存期(OS)的单因素和多因素分析。CI=置信区间;HR=风险比;IPS-E=早期CLL国际预后评分;sBCMA=血清b细胞成熟抗原。
采用多变量模型测试 sBCMA、性别、CLL 国际预后指数 (CLL-IPI) 和早期 CLL 国际预后评分 (IPS-E) 对 TTFT 和 OS 的预测作用。在 CLL-IPI 和 IPS-E 中添加 sBCMA 提高了它们预测 TTFT 和 OS 的预后能力。
总的来说,sBCMA升高强烈提示CLL活跃,在CLL-IPI和IPS-E评分中增加sBCMA的测量,可以提高其预测新诊断患者预后的能力。该研究结果表明,sBCMA可能是一个强大的新的生物标志物来预测新诊断的CLL患者的结果,包括TTFT和OS。如果在更大的数据集中得到验证,sBCMA的确定和确认其在预测CLL患者预后方面的价值将是预测新诊断CLL患者预后能力的一个重大进步。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#预后标志#
103
#淋巴细胞白血病#
63
#标志物#
60
#淋巴细胞#
91
#EMA#
84
#预后标志物#
79
#抗原#
91
写的很好
70