Blood:IGF1R调节肿瘤对PI3K-δ抑制剂的耐药性
2019-04-23 秦启云 MedSci原创
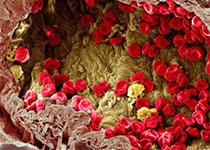
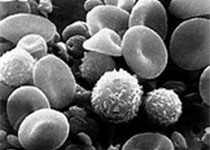
靶向疗法正在彻底改变癌症的治疗,但耐药性极大阻碍了靶向疗法的发展与应用。PI3K-δ抑制剂Idelalisib已被批准用于治疗慢性淋巴细胞白血病(CLL)和非霍奇金淋巴瘤(NHL),但部分患者对其耐药的机制尚不明确。Annika Scheffold等人在小鼠中通过多次肿瘤移植和治疗在体内模拟PI3K-δ抑制剂耐药性的产生。并采用全外显子测序鉴定有无可解释对PI3K-δ抑制剂耐药的频发突变。在小鼠模
Annika Scheffold等人在小鼠中通过多次肿瘤移植和治疗在体内模拟PI3K-δ抑制剂耐药性的产生。并采用全外显子测序鉴定有无可解释对PI3K-δ抑制剂耐药的频发突变。
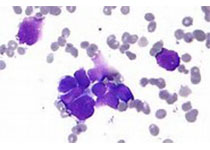
在小鼠模型中,PI3K-δ抑制剂耐药性的产生是由于耐药肿瘤中的胰岛素样生长因子1受体(IFG1R)激活,进而导致了MAPK信号增强。经体外过表达IFG1R,证实了其参与PI3K-δ抑制剂的耐药性。在对PI3K-δ抑制剂耐药的肿瘤中,IFG1R表达上调受FOXO1转录因子和糖原合成酶激酶3β(GSK3B)的功能性激活和核定位增强所调控。
在人类CLL中,高IGF1R表达与12号染色体三体相关。来源于Idelalisib治疗过的患者的CLL细胞,在体外对Idelalisib的敏感性降低;而且经Idelalisib暴露后,MAPK信号增强、IGF1R表达明显上调。
总而言之,本研究表明替代信号级联反应在癌细胞对PI3K-δ抑制剂耐药性产生过程中发挥重要作用,上述信号通路变化或可作为治疗靶点,抑制IGF1R或可作为PI3K-δ抑制剂耐药性肿瘤的补救疗法。
Annika Scheffold,et al.IGF1R as druggable target mediating PI3K-δ inhibitor resistance in a murine model of chronic lymphocytic leukemia. Blood 2019 :blood.2018881029; doi: https://doi.org/10.1182/blood.2018881029
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PI3K-δ抑制剂#
67
#抑制剂#
68
#IGF1R#
94
#IGF#
96
#PI3K#
61
#IGF1#
66