ASCO 2019:AKT抑制剂capivasertib联合氟维司群显著改善HR+HER2-晚期乳腺癌结局
2019-06-08 良医汇-肿瘤医生APP 良医汇-肿瘤医生
2019ASCO于5月31日至6月4日在芝加哥隆重举行,会议期间众多新药研究结果闪亮公布,其中治疗激素受体阳性HER2阴性绝经后晚期乳腺癌的药物AKT抑制剂capivasertib与氟维司群联合,取得了10.3个月的无进展生存,在激素受体阳性晚期乳腺癌众多治疗药物中脱颖而出,有望成为一名新的生力军。会议期间肿瘤资讯有幸采访到中国医学科学院肿瘤医院徐兵河教授,有请徐教授为广大读者介绍FAKTIO
2019ASCO于5月31日至6月4日在芝加哥隆重举行,会议期间众多新药研究结果闪亮公布,其中治疗激素受体阳性HER2阴性绝经后晚期乳腺癌的药物AKT抑制剂capivasertib与氟维司群联合,取得了10.3个月的无进展生存,在激素受体阳性晚期乳腺癌众多治疗药物中脱颖而出,有望成为一名新的生力军。会议期间肿瘤资讯有幸采访到中国医学科学院肿瘤医院徐兵河教授,有请徐教授为广大读者介绍FAKTION研究以及AKT抑制剂capivasertib和氟维司群在晚期乳腺癌治疗中的重要地位。
国家癌症中心/中国医学科学院肿瘤医院内科主任医师
国家新物(抗肿瘤药)临床研究中心主任
中国抗癌协会乳腺癌专业委员会前任主任委员
中国抗癌协会肿瘤药物临床研究专业委员会候任主任委员
国家肿瘤质控中心乳腺癌专家委员会主任委员
国家癌症中心“中国乳腺癌筛查与早诊早治指南”专家委员会主任委员
中国医师协会内科医师分会副会长
中国老年医学学会老年肿瘤分会副会长
北京乳腺病防治学会理事长
北京肿瘤学会副理事长兼秘书长
St.Gallen早期乳腺癌治疗国际共识专家团成员
晚期乳腺癌(ABC)治疗国际共识指南专家团成员
徐兵河教授:HR+晚期乳腺癌有很多治疗手段,如内分泌治疗、内分泌联合靶向治疗等。FAKTION是非常有意义的一项临床研究,共纳入140例既往AI治疗失败的激素受体阳性HER2阴性绝经后晚期乳腺癌患者,随机接受AKT抑制剂capivasertib+氟维司群组或安慰剂+氟维司群治疗。结果显示,主要研究终点两组PFS有显著差别,分别为10.3个月和4.8个月,HR 0.57,单侧和双侧检验的P值分别为0.0017和0.0035。次要研究终点OS也有一定差异,从对照组的20个月延长到capivasertib联合氟维司群组的26个月,有显著改善的趋势,更长时间的随访会得出更明确的结论。作为首个用于HR阳性HER2阴性晚期乳腺癌的AKT抑制剂,capivasertib在FAKTION研究中获得阳性结果,非常令人鼓舞,期望进一步的III期临床研究能再次验证II期结果。
AKT抑制剂在HR阳性晚期乳腺癌中的地位
徐兵河教授:首先明确的是,对于激素受体阳性晚期乳腺癌,内分泌治疗是标准,除非存在内脏危象才首选化疗。选择内分泌治疗的原因在于:(1)副作用小;(2)治疗方便,患者不需要住院也不需要支持治疗,费用相对较低;(3)疗效好,激素受体阳性乳腺癌患者内分泌治疗一旦有效,中位PFS可达1年,而化疗通常为4~6个月。其次,内分泌治疗既可选择单药,也可联合治疗,目前趋势是内分泌联合靶向治疗,如内分泌联合CDK4/6抑制剂,与内分泌单药治疗相比,可显著延长PFS,这一进步具有划时代的意义。
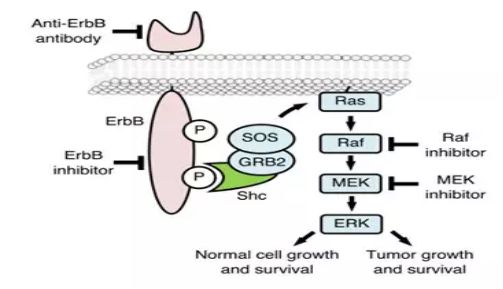
除CDK4/6抑制剂外,FAKTION研究中的AKT抑制剂与内分泌药物氟维司群联合也取得了很好的疗效,AKT抑制剂作用于PI3K/AKT/PTEN通路,该通路活化后导致激素受体阳性乳腺癌内分泌治疗耐药。体外研究证实,抑制该通路并与内分泌治疗联合具有协同作用,并能克服耐药,FAKTION研究结果也证实了AKT抑制剂capivasertib联合氟维司群比单用氟维司群治疗AI耐药患者,可显著延长PFS,同时还有改善OS的趋势。其他与内分泌治疗联合使用的药物也在探索中,如PI3Kα抑制剂,SOLAR-1研究显示,PI3Kα抑制剂联合氟维司群治疗AI耐药患者,PFS也有显著改善。
个人认为,AKT抑制剂联合内分泌治疗的疗效至少与CDK4/6抑制剂联合内分泌治疗疗效相当,但CDK4/6抑制剂的一些副作用,如骨髓抑制、白细胞下降使得部分患者不能耐受,而AKT抑制剂的副作用与CDK4/6抑制剂不同,为患者提供了更多更好的治疗选择。PI3Kα抑制剂同样存在较大副作用,如高血糖,常常导致患者停药。而且PI3Kα抑制剂只对PIK3CA基因突变患者有效,此类患者仅占30%左右。从FAKTION研究可以看出,突变与否并不影响AKT抑制剂疗效,因此适用人群更广。
氟维司群在内分泌联合靶向治疗中的地位
徐兵河教授:乳腺癌内分泌治疗从最初的他莫昔芬到芳香化酶抑制剂,再到雌激素受体下调剂氟维司群,历经数十年的变迁。研究结果显示,氟维司群疗效至少与AI相似,在某些方面更优,如既往未行辅助内分泌治疗患者复发转移后,使用氟维司群治疗的疗效优于AI;辅助治疗使用过AI的患者,复发转移后首选氟维司群一线治疗。氟维司群一月一次使用方便;有些患者使用AI类药物可导致肌肉关节疼痛而难以耐受,氟维司群则没有这类副作用。总体而言,氟维司群安全性更好,使用方便,疗效明确,所以在激素受体阳性绝经后晚期乳腺癌患者中氟维司群的地位非常明确,绝经前患者可以在去势基础上使用氟维司群。
氟维司群不但作为单药治疗疗效好,而且特别适合与靶向药物联合发挥更大的治疗作用,如与CDK4/6抑制剂联合在二线人群中,中位PFS从6个月延长到12个月;对于辅助治疗中使用过AI类药物的晚期乳腺癌患者,一线氟维司群联合CDK4/6抑制剂或AKT抑制剂,患者获益可能更突出,期待这一推论能够得到进一步的研究结果证实。同时,氟维司群联合靶向治疗使用方便,一月一次肌肉注射联合口服的靶向药物,患者容易接受。
激素受体阳性晚期乳腺癌治疗方案选择
徐兵河教授:过去认为,激素受体阳性乳腺癌肿瘤负荷较大或存在内脏危象时,单用内分泌治疗起效慢。现在已进入了内分泌联合靶向治疗时代,过去的一些观念要相应发生改变,因为内分泌与靶向治疗联合后疗效提高,起效也更快,所以过去认为不适合内分泌治疗的部分患者现在可以考虑探索内分泌联合靶向治疗,争取给患者创造内分泌治疗的机会,通常越早内分泌联合治疗患者获益越大。
此外激素受体阳性患者选择哪种内分泌治疗药物也需要仔细推敲,如果患者既往未使用过AI类药物可以选择AI类药物或是氟维司群,但如果使用过AI类药物,氟维司群就应作为首选考虑,或是患者耐受不了AI类药物副作用,氟维司群亦作为优选。个人认为,只要在患者经济允许并能耐受情况下,内分泌治疗联合靶向治疗应该作为最重要的选择加以考虑。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Akt#
51
#ASC#
44
#CAP#
48
#抑制剂#
54
#HER2-#
65
#capivasertib#
51