JACC:单动脉冠脉搭桥预后劣于多动脉搭桥
2019-10-31 不详 MedSci原创
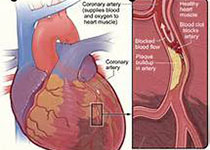
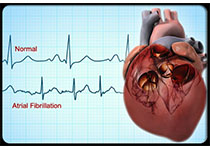
多动脉和单动脉冠脉搭桥(CABG)的收益比较一直存在争议。本研究的目的旨在评估和比较多动脉和单动脉CABG术后的远期生存率、并发症和搭桥的通畅性。本研究共纳入分析了2005-2012年接受CABG治疗的26124名患者,其中3647(14%)名患者接受了多动脉CABG,与多动脉CABG相比,单动脉CABG患者年龄更大(平均68 vs. 61岁; p < 0.001),并发症更多,接受更少的旁
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#搭桥#
72
#JACC#
54
#ACC#
95
#冠脉搭桥#
101