JCO:BGJ398治疗FGFR改变晚期胆管癌
2017-11-29 MedSci MedSci原创
对于一线吉西他滨治疗失败的胆管癌患者尚无标准治疗方法。FGFR融合/易位约在13%-17%肝内胆管癌中出现。BGJ398是一种口服的选择性pan-FGFR酶抑制剂,在临床前实验中对FGFR改变肿瘤具有治疗效果。JCO近期发表了一篇文章,研究BGJ398治疗FGFR改变胆管癌患者的临床疗效。
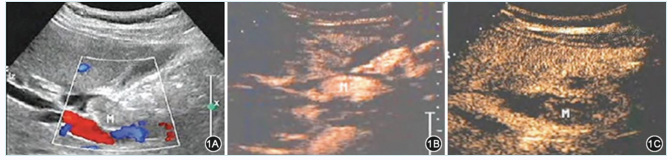
对于一线吉西他滨治疗失败的胆管癌患者尚无标准治疗方法。FGFR融合/易位约在13%-17%肝内胆管癌中出现。BGJ398是一种口服的选择性pan-FGFR酶抑制剂,在临床前实验中对FGFR改变肿瘤具有治疗效果。JCO近期发表了一篇文章,研究BGJ398治疗FGFR改变胆管癌患者的临床疗效。研究纳入的患者为接受过治疗且疾病出现进展的晚期或转移性含有FGFR2融合或其他FGFR改变的晚期或转移性胆管癌患者,评估BGJ398在这些患者中的抗肿瘤活性。患者每天接受BGJ398 125mg治疗,持续21天,而后间歇7天(28天一个周期)。主要的研究终点为总反应率。研究共纳入61例FGFR融合(n=48),突变(n=8)或扩增(n=3)的患者。在数据收集截止时,50例患者中断治疗。所有有治疗反应的肿瘤含有FGFR2融合。总反应率14.8%(仅有FGFR2融合为18.8%),疾病控制率为75.4%(仅有FGFR2融合为83.3%),平均无进展生存期为5.8个月。不良反应包括高磷血症(72.1%),虚弱(36.1%),口腔炎(29.5%)和脱发(26.2%)。25例患者出现3级或4级治疗相关不良反应,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCO#
59
#FGFR#
78
#GFR#
59
#胆管#
77
学习了!受益匪浅
81
学习啦!谢谢分享!学习啦!谢谢分享!
107